Thrombotic Thrombocytopenic Purpura
Summary
Thrombotic thrombocytopenic purpura (TTP) is a life-threatening thrombotic microangiopathy (TMA) caused by severe deficiency of ADAMTS13, the von Willebrand factor (vWF)-cleaving protease. This leads to accumulation of ultra-large vWF multimers, causing platelet aggregation, microvascular thrombosis, and microangiopathic haemolytic anaemia (MAHA). TTP can be acquired (autoimmune anti-ADAMTS13 antibodies, most common in adults) or congenital (Upshaw-Schulman syndrome, inherited ADAMTS13 deficiency). The classic pentad (thrombocytopenia, MAHA, neurological symptoms, fever, renal impairment) is rarely complete. Without treatment, TTP is rapidly fatal. Emergency plasma exchange (PEX) is life-saving and should not be delayed for confirmatory testing. Modern additions include caplacizumab (anti-vWF nanobody) and rituximab.
Key Facts
- Definition: TMA with ADAMTS13 activity less than 10% (acquired or congenital)
- Incidence: 3-10 per million per year
- Mortality: Untreated >90%; with PEX 10-20%
- Peak Demographics: Adults 20-50 years; F > M (2:1)
- Pathognomonic: ADAMTS13 less than 10% + schistocytes on blood film
- Gold Standard Investigation: ADAMTS13 activity level
- First-line Treatment: Emergency plasma exchange + steroids + caplacizumab
- Prognosis: With treatment, 80-90% survival; relapse 30-50%
Clinical Pearls
Diagnostic Pearl: Thrombocytopenia + MAHA (schistocytes) = TMA until proven otherwise. Use PLASMIC score for pretest probability.
Emergency Pearl: DO NOT delay plasma exchange waiting for ADAMTS13 result - mortality rises each day untreated.
Pitfall Warning: NEVER transfuse platelets in TTP - they "add fuel to the fire" and worsen thrombosis.
Mnemonic: TTP Pentad - Thrombocytopenia, Trauma to red cells (MAHA), Pyrexia, Trouble thinking (neuro), Pee problems (renal)
Why This Matters Clinically
TTP is a haematological emergency. Rapid recognition and immediate plasma exchange saves lives. Delay of even hours increases mortality. Caplacizumab has transformed outcomes. This is a core MRCP and acute medicine topic.
Incidence
- 3-10 per million per year
- Acquired TTP accounts for 95% of adult cases
- Congenital: less than 5%
Demographics
| Factor | Details |
|---|---|
| Age | Peak 20-50 years |
| Sex | F:M 2:1 |
| Ethnicity | African Americans 3x higher incidence |
Risk Factors / Triggers
| Trigger | Mechanism |
|---|---|
| Infection | Immune trigger for antibody formation |
| Pregnancy | Acquired TTP or unmasking congenital |
| Autoimmune disease (SLE) | Associated |
| HIV | Increased risk |
| Drugs (ticlopidine, quinine, rarely clopidogrel) | Drug-induced TTP |
| Bone marrow transplant | Secondary TMA |
Normal ADAMTS13 Function
- ADAMTS13 cleaves ultra-large vWF multimers into smaller fragments
- Prevents excessive platelet adhesion
Mechanism in TTP
Step 1: ADAMTS13 Deficiency
- Acquired: Autoantibodies (IgG) against ADAMTS13
- Congenital: Mutations in ADAMTS13 gene
Step 2: Accumulation of Ultra-Large vWF Multimers
- Uncleaved vWF multimers released from endothelium
- Highly thrombogenic
Step 3: Platelet Aggregation
- Platelets adhere to ultra-large vWF
- Microvascular platelet-rich thrombi form
- Platelet consumption → thrombocytopenia
Step 4: Microangiopathic Haemolysis
- RBCs sheared by fibrin strands in microvasculature
- Schistocytes (fragmented RBCs) on blood film
- Elevated LDH, low haptoglobin, unconjugated hyperbilirubinaemia
Step 5: End-Organ Ischaemia
- Brain: Confusion, seizures, stroke, coma
- Heart: Ischaemia, MI
- Kidney: Mild impairment (unlike HUS where severe)
Classification
| Type | Mechanism | ADAMTS13 Activity |
|---|---|---|
| Acquired immune TTP | Anti-ADAMTS13 antibodies | less than 10% |
| Congenital (Upshaw-Schulman) | ADAMTS13 gene mutation | less than 10% |
| Secondary TMA | Various (drugs, transplant, pregnancy) | Often >10% |
Symptoms
Signs
Classic Pentad (Rarely Complete)
- Thrombocytopenia (100%)
- MAHA with schistocytes (100%)
- Neurological symptoms (60-70%)
- Fever (25%)
- Renal impairment (mild, less than 25%)
Red Flags
[!CAUTION]
- Any TMA with neurological features
- Cardiac ischaemia with thrombocytopenia
- Pregnancy with TMA
- PLASMIC score ≥5
Blood Film (Essential)
- Schistocytes (fragmented RBCs) - >1% is significant
- Polychromasia
- Reduced platelets
Laboratory
| Test | Finding | Notes |
|---|---|---|
| Platelets | Very low (often less than 30 x10⁹/L) | Severe thrombocytopenia |
| Haemoglobin | Low | MAHA |
| Reticulocytes | Elevated | Haemolysis |
| LDH | Very elevated | Haemolysis marker |
| Haptoglobin | Undetectable | Consumed in haemolysis |
| Bilirubin | Elevated (unconjugated) | Haemolysis |
| Direct Coombs | Negative | Distinguishes from AIHA |
| Creatinine | Mildly elevated or normal | Unlike HUS |
| Coagulation (PT, APTT) | Normal | Distinguishes from DIC |
ADAMTS13
| Test | Interpretation |
|---|---|
| ADAMTS13 activity | less than 10% diagnostic of TTP |
| ADAMTS13 inhibitor | Positive in acquired (antibody) |
| ADAMTS13 antibody | Confirms immune-mediated |
Take sample BEFORE plasma exchange/transfusion
PLASMIC Score (Pretest Probability)
| Variable | Points |
|---|---|
| Platelet count less than 30 | +1 |
| Haemolysis variables present | +1 |
| No active cancer | +1 |
| No stem cell or organ transplant | +1 |
| MCV less than 90 fL | +1 |
| INR less than 1.5 | +1 |
| Creatinine less than 177 μmol/L (2 mg/dL) | +1 |
Score ≥6: High probability (72% have ADAMTS13 less than 10%)
Algorithm
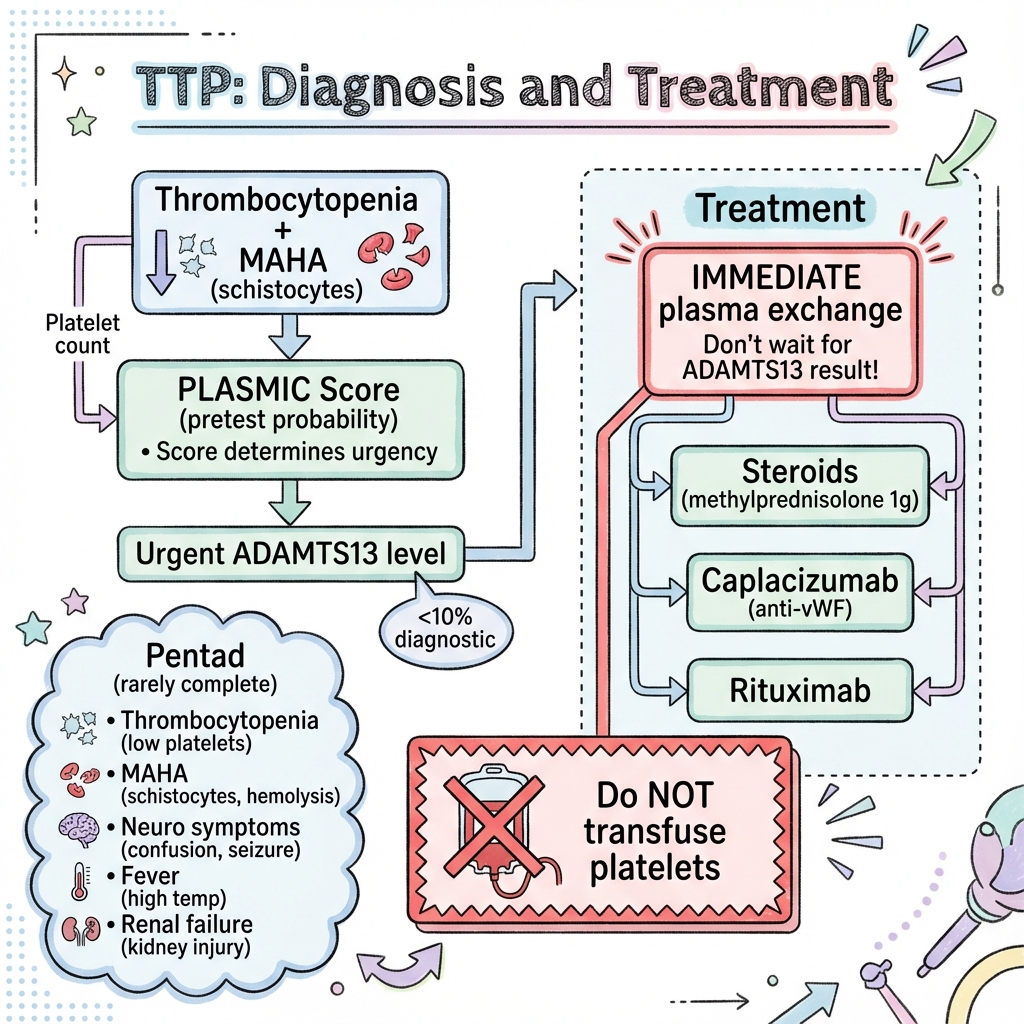
Emergency Treatment (Start Immediately)
DO NOT wait for ADAMTS13 result if clinical suspicion high
| Treatment | Details |
|---|---|
| Plasma exchange (PEX) | 1.5 plasma volumes daily; removes autoantibodies and ultra-large vWF, replaces ADAMTS13 |
| Corticosteroids | Methylprednisolone 1g IV daily x3 then prednisone 1mg/kg |
| Caplacizumab | 11mg IV then 11mg SC daily; anti-vWF nanobody - prevents vWF-platelet interaction |
Second-Line / Refractory
| Treatment | Indication |
|---|---|
| Rituximab | Standard addition; 375mg/m² weekly x4; reduces relapse |
| Twice daily PEX | Refractory disease |
| Ciclosporin | Refractory |
| Bortezomib | Refractory |
| Splenectomy | Rarely indicated now |
Supportive Care
- Red cell transfusion as needed
- NO PLATELET TRANSFUSION (unless life-threatening bleeding)
- Folic acid
- VTE prophylaxis once platelets recover
Monitoring Response
- Daily platelet count, LDH
- Aim: Platelet count >150 x2 consecutive days
- Then can stop PEX
- Continue caplacizumab for 30 days post-last PEX
- Monitor ADAMTS13 to confirm recovery and guide relapse risk
Prevention of Relapse
- Rituximab reduces relapse (30-50% → 10-15%)
- Monitor ADAMTS13 activity during remission
- Preemptive rituximab if ADAMTS13 falling
| Complication | Incidence | Management |
|---|---|---|
| Stroke | 10-20% | Acute stroke care |
| Myocardial infarction | 5-10% | Cardiology |
| Death | 10-20% with treatment | Early aggressive therapy |
| Relapse | 30-50% | Rituximab, monitoring |
| PEX complications | Line infection, citrate toxicity | Careful management |
Outcomes
- With PEX: 80-90% survival (previously >90% mortality)
- With PEX + caplacizumab: Faster response, fewer refractory cases
- Relapse rate: 30-50% (reduced with rituximab)
Prognostic Factors
Good:
- Early treatment
- Response to PEX within 5 days
- ADAMTS13 recovery
Poor:
- Cardiac involvement
- Refractory disease
- Delayed diagnosis
Key Guidelines
- ISTH Guidelines on TMA (2020) — Diagnosis and management PMID: 32239796
- BSH Guidelines on TTP (2012/2023 update) — UK practice
Key Trials
TITAN Trial (2016) — Caplacizumab + PEX vs PEX alone; faster platelet recovery, fewer exacerbations. PMID: 26833331
HERCULES Trial (2019) — Confirmed caplacizumab benefit; reduced TTP-related death, exacerbation, recurrence. PMID: 30625035
What is TTP?
Your blood is forming tiny clots in small blood vessels throughout your body. This uses up your platelets (a type of blood cell) and damages your red blood cells. It can affect your brain, heart, and other organs.
How is it treated?
The main treatment is plasma exchange - we filter your blood and replace the plasma to remove the harmful antibodies. You'll also receive other medications to help.
Warning Signs
Return if: Headache, confusion, chest pain, bleeding.
-
Scully M et al. Caplacizumab treatment for acquired thrombotic thrombocytopenic purpura (HERCULES). N Engl J Med. 2019;380(4):335-346. PMID: 30625035
-
Peyvandi F et al. Caplacizumab for Acquired Thrombotic Thrombocytopenic Purpura (TITAN). N Engl J Med. 2016;374(6):511-522. PMID: 26833331
-
Cuker A et al. PLASMIC score. Lancet Haematol. 2017;4(4):e157-e164. PMID: 28259520
-
Scully M et al. Guidelines on the diagnosis and management of TTP. Br J Haematol. 2012;158(3):323-335. PMID: 22624596
-
Zheng XL et al. ISTH guidelines for treatment of TTP. J Thromb Haemost. 2020;18(10):2496-2502. PMID: 32239796
Viva Points
"TTP is a TMA caused by ADAMTS13 deficiency (less than 10%). Presents with thrombocytopenia, MAHA, neurological symptoms. Emergency: plasma exchange immediately. Add steroids, caplacizumab, rituximab. NO platelet transfusion."
Key Facts
- ADAMTS13 less than 10% = TTP
- PLASMIC score to assess probability
- PEX is lifesaving - do not delay
- Never transfuse platelets (worsens thrombosis)
- Caplacizumab (HERCULES trial) improves outcomes
Common Mistakes
- ❌ Transfusing platelets
- ❌ Waiting for ADAMTS13 to start PEX
- ❌ Missing diagnosis (TMA = TTP until proven otherwise)
Last Reviewed: 2026-01-01 | MedVellum Editorial Team