Phaeochromocytoma
Summary
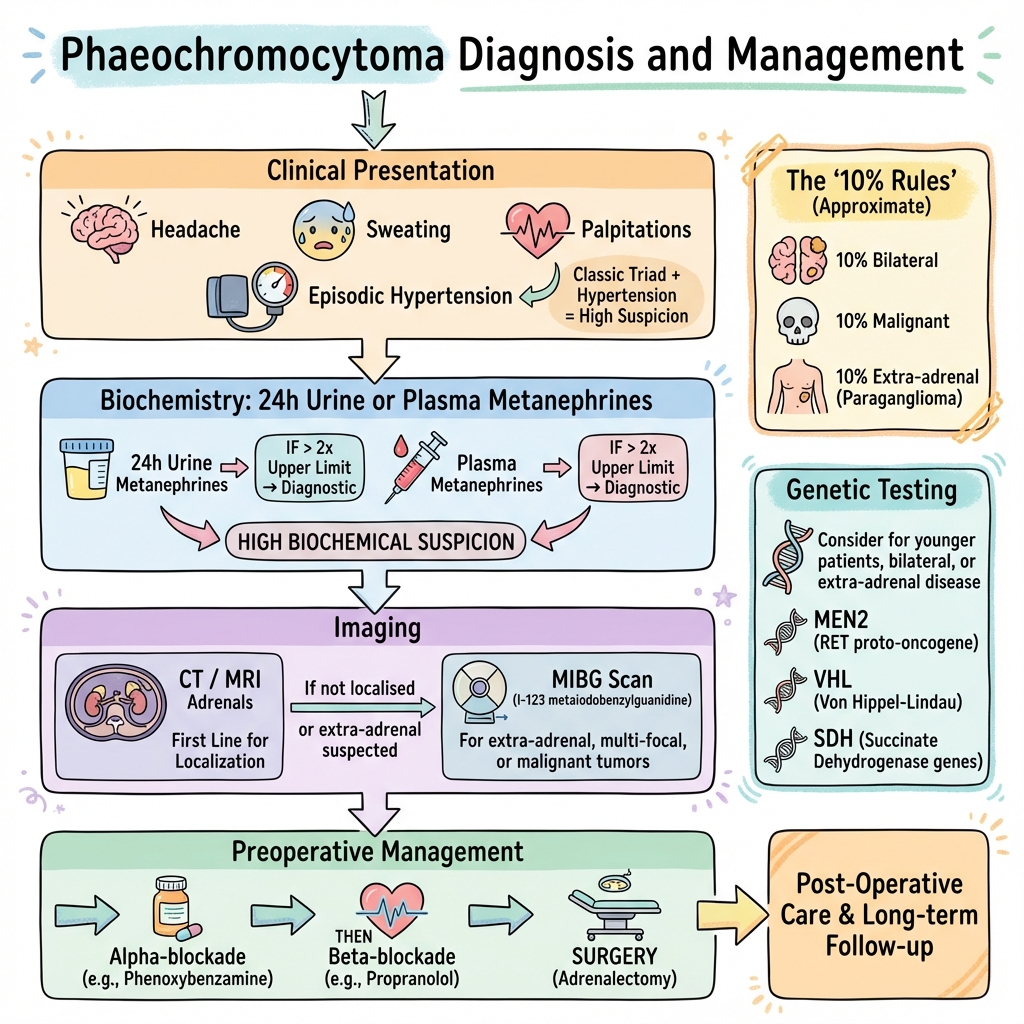
Phaeochromocytoma is a rare catecholamine-secreting tumour arising from chromaffin cells of the adrenal medulla. When arising from extra-adrenal sympathetic ganglia, it is termed paraganglioma. These tumours produce excess adrenaline and noradrenaline, causing paroxysmal or sustained hypertension, headaches, sweating, and palpitations. Although classically described by the 10 percent rules (10% bilateral, malignant, extra-adrenal, familial), genetic testing has revealed hereditary syndromes (MEN2, VHL, SDH mutations) in up to 40%. Diagnosis is by measuring plasma or urinary metanephrines. Treatment requires careful preoperative alpha-blockade followed by beta-blockade before surgical resection.
Key Facts
- Definition: Catecholamine-secreting tumour of adrenal medulla (or paraganglia)
- Incidence: 2-8 per million per year
- Peak Demographics: 30-50 years
- Classical Triad: Headache, sweating, palpitations (during paroxysms)
- Pathognomonic: Plasma metanephrines more than 2x upper limit
- Gold Standard Investigation: Plasma or 24h urine metanephrines
- First-line Treatment: Alpha-blockade then beta-blockade, then surgical resection
- Prognosis: 90% cured by surgery; 10% malignant
Clinical Pearls
Diagnostic Pearl: The 5 Ps - Pressure (hypertension), Pain (headache), Perspiration, Palpitations, Pallor
Treatment Pearl: ALWAYS alpha-block before beta-block. Beta-blockade alone causes unopposed alpha stimulation and hypertensive crisis.
Emergency Pearl: Phaeochromocytoma crisis is managed with IV phentolamine (alpha-blocker), NOT beta-blockers.
Why This Matters Clinically
Phaeochromocytoma is a curable cause of hypertension. Missing it can lead to hypertensive crisis during surgery or pregnancy. All adrenal incidentalomas require biochemical screening.
Incidence
- 2-8 per million per year
- Found in 0.1-0.6% of hypertensive patients
- 4% of adrenal incidentalomas
The 10 Percent Rules (Updated)
| Rule | Details |
|---|---|
| 10% bilateral | Higher in familial syndromes |
| 10% malignant | 10-15% |
| 10% extra-adrenal | Paragangliomas |
| 10% familial | Now known to be up to 40% hereditary |
| 10% normotensive | Rare, usually dopamine-secreting |
Hereditary Syndromes
| Syndrome | Gene | Features |
|---|---|---|
| MEN2A/2B | RET | Medullary thyroid cancer, hyperparathyroidism |
| VHL | VHL | Haemangioblastomas, renal cell carcinoma |
| NF1 | NF1 | Neurofibromas, cafe-au-lait spots |
| SDH mutations | SDHB, SDHD | High malignancy risk (SDHB) |
Mechanism
Step 1: Tumour Origin
- Arises from chromaffin cells (adrenal medulla) or paraganglia
- Chromaffin cells derive from neural crest
Step 2: Catecholamine Synthesis
- Tumour produces excess noradrenaline, adrenaline (or rarely dopamine)
- Stored in granules, released episodically or continuously
Step 3: Catecholamine Effects
- Alpha-1 receptors: Vasoconstriction leads to hypertension
- Beta-1 receptors: Increased heart rate, contractility
- Beta-2 receptors: Vasodilation (can cause hypotension in adrenaline-secreting tumours)
- Metabolic: Hyperglycaemia, lipolysis
Step 4: Clinical Manifestations
- Paroxysmal or sustained hypertension
- Sympathetic activation symptoms
- Metabolic derangements
Catecholamine Metabolism
- Catecholamines metabolised to metanephrines and VMA
- Metanephrines continuously produced within tumour (more sensitive marker)
Classical Triad (during paroxysm)
Other Symptoms
Signs
Paroxysms
Red Flags
[!CAUTION]
- Young patient with hypertension
- Resistant hypertension (more than 3 drugs)
- Hypertension with adrenal mass
- Episodic symptoms with hypertension
- Family history of MEN2/VHL/NF1
Assessment
General:
- Blood pressure (may be labile)
- Postural BP
Skin:
- Cafe-au-lait spots (NF1)
- Neurofibromas (NF1)
Neck:
- Thyroid nodules (MEN2)
Abdominal:
- Rarely palpable mass
Ophthalmology:
- Retinal haemangioblastomas (VHL)
Biochemistry
| Test | Interpretation |
|---|---|
| Plasma metanephrines | More than 2x upper limit is highly suggestive |
| 24h urine metanephrines | Alternative; more than 2x upper limit |
| Plasma catecholamines | Less sensitive; stress affects |
| Chromogranin A | Elevated in neuroendocrine tumours |
Imaging
| Modality | Use |
|---|---|
| CT Adrenals | First-line imaging; high sensitivity |
| MRI | Light bulb sign on T2; better for extra-adrenal |
| MIBG scan | Functional imaging; if CT/MRI inconclusive |
| PET (Ga-DOTATATE) | If MIBG negative; metastatic workup |
Genetic Testing
- Recommended for ALL patients (up to 40% hereditary)
- SDH mutations, RET, VHL, NF1
Algorithm
Preoperative Preparation (Essential)
Step 1: Alpha-blockade FIRST (2-4 weeks before surgery)
- Phenoxybenzamine 10mg BD, increase to 20-40mg BD
- OR Doxazosin 2-16mg daily
Step 2: Volume expansion
- High salt diet
- IV fluids if needed
Step 3: Beta-blockade (only after adequate alpha-block)
- Propranolol or atenolol
- NEVER give beta-blocker alone (hypertensive crisis)
Step 4: Surgery
- Laparoscopic adrenalectomy (preferred)
- Close intraoperative BP monitoring
- Have phentolamine ready
Hypertensive Crisis
- IV phentolamine (alpha-blocker)
- IV nitroprusside
- Avoid beta-blockers alone
Malignant Phaeochromocytoma
- Surgery if resectable
- MIBG therapy (I-131)
- Chemotherapy (CVD regimen)
- Targeted therapy (sunitinib)
| Complication | Management |
|---|---|
| Hypertensive crisis | Phentolamine, nitroprusside |
| Stroke, MI | Prevention with preop alpha-block |
| Intraoperative hypotension | Volume, vasopressors |
| Metastatic disease | MIBG, chemotherapy |
Outcomes
- 90% cure with surgical resection
- 10-15% malignant (metastatic)
- Malignant: 5-year survival 50%
- Lifelong follow-up required (recurrence)
Key Guidelines
- Endocrine Society Guidelines (2014) — Phaeochromocytoma and paraganglioma PMID: 24893135
What is Phaeochromocytoma?
A rare tumour of the adrenal gland that produces too much adrenaline. This causes high blood pressure, headaches, sweating, and a fast heartbeat.
How is it treated?
Surgery to remove the tumour. Before surgery, you will take medications to control your blood pressure safely.
-
Lenders JWM et al. Pheochromocytoma and Paraganglioma: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2014;99(6):1915-1942. PMID: 24893135
-
Neumann HPH et al. Pheochromocytoma. N Engl J Med. 2019;381(6):552-565. PMID: 31390501
-
Pacak K et al. Recent advances in genetics, diagnosis, and treatment of pheochromocytoma. Ann Intern Med. 2001;134(4):315-329. PMID: 11182843
Viva Points
"Phaeochromocytoma is a catecholamine-secreting adrenal tumour. Diagnose with plasma/urine metanephrines. The triad is headache, sweating, palpitations. Treatment: alpha-block FIRST, then beta-block, then surgery. Up to 40% are hereditary - test all patients."
Key Facts
- Plasma metanephrines most sensitive test
- Alpha-block before beta-block (ALWAYS)
- 40% hereditary (MEN2, VHL, SDH, NF1)
- 10-15% malignant
Common Mistakes
- Beta-blocker without alpha-blockade
- Not screening adrenal incidentalomas
- Forgetting genetic testing
Last Reviewed: 2026-01-01 | MedVellum Editorial Team