Pulmonary Embolism
Summary
Pulmonary embolism (PE) is a potentially life-threatening condition caused by obstruction of the pulmonary arteries, usually by thromboembolism from deep veins of the legs. Clinical presentation ranges from asymptomatic to sudden death, with classic features of dyspnoea, pleuritic chest pain, and tachycardia. Diagnosis uses clinical probability scoring (Wells, Geneva) followed by D-dimer in low-risk patients or CTPA in higher-risk patients. Risk stratification using PESI score and RV function assessment guides management. Treatment is anticoagulation (DOACs preferred), with thrombolysis reserved for haemodynamically unstable patients.
Key Facts
- Definition: Obstruction of pulmonary arteries by thrombus
- Incidence: 60-70 per 100,000 per year
- Peak Demographics: Increases with age; risk factors crucial
- Pathognomonic: Clinical suspicion + CTPA-confirmed filling defect
- Gold Standard Investigation: CTPA
- First-line Treatment: Anticoagulation (DOACs preferred)
- Prognosis: Low risk 1% mortality; massive PE 30%+ mortality
Clinical Pearls
Diagnostic Pearl: Wells score PE-unlikely (less than 4) + negative D-dimer = PE safely excluded.
Risk Stratification Pearl: sPESI 0 identifies truly low-risk patients suitable for outpatient treatment.
Thrombolysis Pearl: Reserve for haemodynamically unstable (massive) PE - half-dose for borderline cases debated.
| Category | Examples |
|---|---|
| Provoked | Surgery, immobility, trauma, pregnancy |
| Unprovoked | Cancer, thrombophilia, unknown |
| Strong | Major surgery, fracture, hospital admission |
| Moderate | Hormonal therapy, cancer |
- Dyspnoea (most common)
- Pleuritic chest pain
- Tachycardia
- Haemoptysis
- Syncope (massive PE)
- Leg swelling (concurrent DVT)
Wells Score
| Variable | Points |
|---|---|
| Clinical signs of DVT | 3 |
| PE most likely diagnosis | 3 |
| Tachycardia greater than 100 | 1.5 |
| Immobilisation/surgery | 1.5 |
| Previous DVT/PE | 1.5 |
| Haemoptysis | 1 |
| Malignancy | 1 |
- Less than 4 = PE unlikely
- 4 or more = PE likely
Pathway
- PE unlikely + negative D-dimer = excluded
- PE likely OR positive D-dimer = CTPA
Algorithm
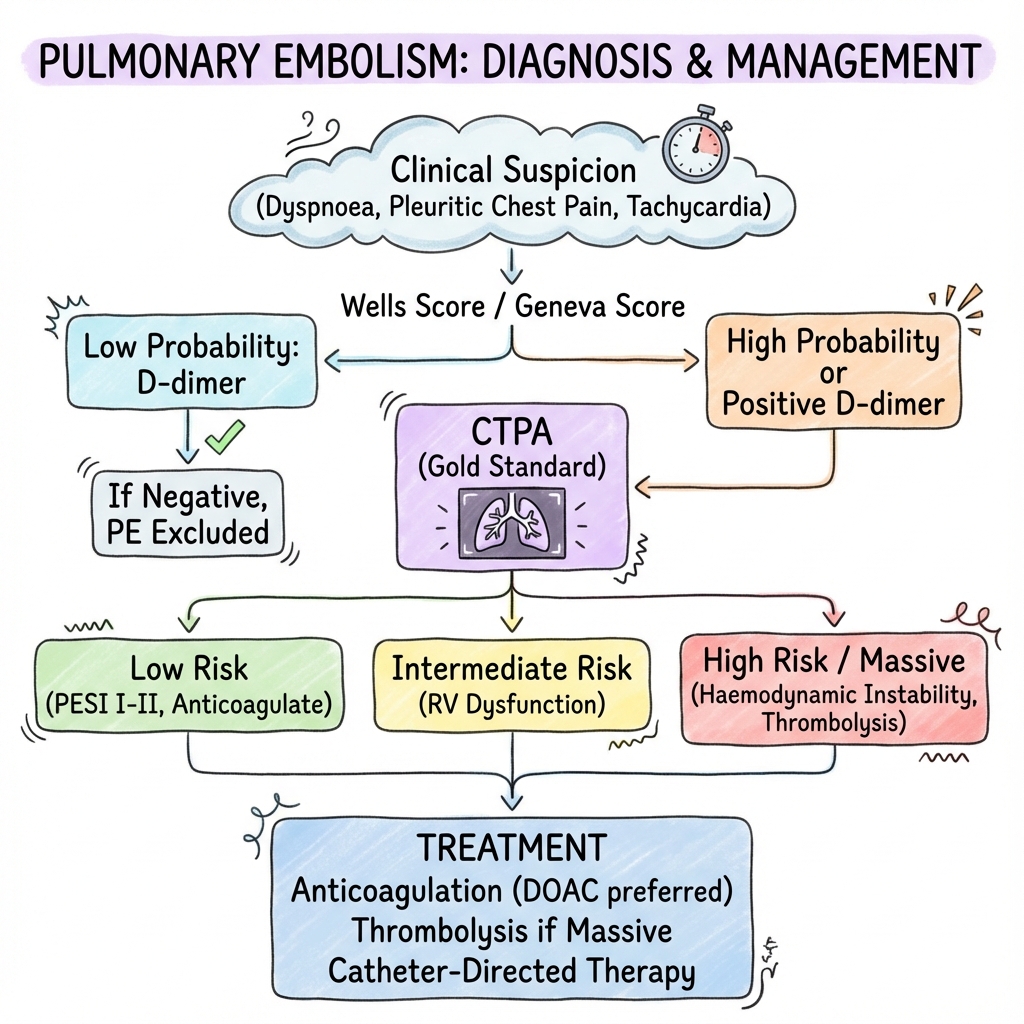
Risk Stratification (ESC)
| Risk | Criteria | Management |
|---|---|---|
| Low | sPESI 0, no RV dysfunction | Outpatient DOAC |
| Intermediate-low | sPESI 1+, RV dysfunction OR biomarkers elevated | Ward, anticoagulate |
| Intermediate-high | RV dysfunction AND biomarkers elevated | Consider thrombolysis if deterioration |
| High | Haemodynamic instability | Thrombolysis or catheter therapy |
Anticoagulation
| Drug | Regimen |
|---|---|
| Apixaban | 10mg BD x7 days, then 5mg BD |
| Rivaroxaban | 15mg BD x21 days, then 20mg OD |
| LMWH/Warfarin | Alternative |
Thrombolysis
| Drug | Dose |
|---|---|
| Alteplase | 100mg over 2h (or 50mg if intermediate-high) |
-
Konstantinides SV et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2020;41(4):543-603. PMID: 31504429
-
van Es N et al. Validated clinical prediction rules for PE. Ann Intern Med. 2016;165(4):253-261. PMID: 27182696
Viva Points
"PE: thrombus in pulmonary arteries. Wells score + D-dimer or CTPA. Risk stratify with sPESI/RV function. Low risk = DOAC outpatient. High risk/massive = thrombolysis. ESC 2019 guidelines."
Last Reviewed: 2026-01-01 | MedVellum Editorial Team