Myasthenia Gravis
Summary
Myasthenia gravis (MG) is an autoimmune disorder of the neuromuscular junction (NMJ) characterised by fluctuating fatigable weakness of skeletal muscles. The most common form involves autoantibodies against the acetylcholine receptor (AChR) at the postsynaptic membrane, impairing neuromuscular transmission. Clinically, MG presents with ptosis, diplopia, bulbar weakness (dysarthria, dysphagia), and limb weakness that worsens with activity and improves with rest. Diagnosis is confirmed by antibody testing, electrophysiology (decremental response on repetitive nerve stimulation), and response to acetylcholinesterase inhibitors. Thymoma is associated in 10-15%. Treatment includes symptomatic therapy (pyridostigmine), immunosuppression (steroids, azathioprine), and thymectomy. Myasthenic crisis (respiratory failure) is a life-threatening emergency requiring ICU care, IVIG, or plasma exchange.
Key Facts
- Definition: Autoimmune NMJ disorder with anti-AChR or anti-MuSK antibodies
- Incidence: 10-20 per million per year
- Peak Demographics: Bimodal - women 20-40, men 60-80
- Pathognomonic: Fluctuating fatigable weakness improving with rest
- Gold Standard Investigation: AChR antibodies (85% sensitive in generalised MG)
- Thymoma Association: 10-15%
- First-line Treatment: Pyridostigmine (symptomatic) + steroids/immunosuppression
- Prognosis: Good with treatment; mortality now less than 5%
Clinical Pearls
Diagnostic Pearl: If AChR antibodies negative in generalised MG, test for MuSK antibodies (5-10% of seronegative cases).
Treatment Pearl: When starting steroids in MG, start LOW and SLOW - high doses can initially worsen weakness.
Emergency Pearl: Distinguish MG crisis (weakness, ptosis, sweating, tachycardia) from cholinergic crisis (excessive secretions, bradycardia, miosis) - stop pyridostigmine in latter.
Why This Matters Clinically
MG is a treatable cause of fatigable weakness. Failure to recognise can lead to respiratory failure. Understanding the approach to MG crisis is critical for acute medicine and ICU.
Incidence and Prevalence
- Incidence: 10-20 per million per year
- Prevalence: 150-200 per million
- Increasing due to ageing population and improved diagnosis
Demographics
| Factor | Details |
|---|---|
| Age | Bimodal: 20-40 (women), 60-80 (men) |
| Sex | F:M 3:2 in young; M:F 1.5:1 in elderly |
| Thymoma | 10-15% of MG patients |
Classification
| Type | Antibody | Features |
|---|---|---|
| AChR-positive | Anti-AChR (85%) | Most common; responds to all treatments |
| MuSK-positive | Anti-MuSK (5-10%) | Bulbar predominant; atrophy; poor response to pyridostigmine |
| LRP4-positive | Anti-LRP4 (1-3%) | Milder phenotype |
| Seronegative | None detected (5-10%) | May have low-affinity antibodies |
Mechanism
Step 1: Loss of Immune Tolerance
- Thymus abnormality (hyperplasia or thymoma) in 75%
- Autoreactive T and B cells activated
- Antibody production against NMJ components
Step 2: Antibody Binding
AChR antibodies:
- Bind to AChR at postsynaptic membrane
- Receptor internalisation and degradation
- Complement-mediated destruction of postsynaptic membrane
- Reduced AChR density
MuSK antibodies:
- Bind to muscle-specific kinase
- Disrupts AChR clustering (MuSK organises AChR aggregation)
- No complement activation
- Different clinical phenotype
Step 3: Impaired Neuromuscular Transmission
- Reduced safety factor for transmission
- Under normal conditions: ACh release exceeds threshold
- With exercise: ACh release declines, falls below threshold
- Results in fatigable weakness
Step 4: Clinical Manifestations
- Ocular muscles most susceptible (small motor units)
- Bulbar muscles (swallowing, speech)
- Limb muscles (proximal greater than distal)
- Respiratory muscles (life-threatening)
Thymus Pathology
| Pathology | Frequency | Notes |
|---|---|---|
| Thymic hyperplasia | 60% | Germinal centres |
| Thymoma | 10-15% | May be malignant |
| Normal/atrophic | 25% | More common in elderly |
Symptoms
Ocular (85% at presentation):
Bulbar:
Limb:
Respiratory:
Key Feature: Fluctuation
Signs
Classification (MGFA)
| Class | Description |
|---|---|
| I | Ocular only |
| II | Mild generalised |
| III | Moderate generalised |
| IV | Severe generalised |
| V | Intubation required (crisis) |
Red Flags (MG Crisis)
[!CAUTION]
- FVC less than 1L or declining
- Unable to count to 20 in one breath
- Increasing dyspnoea
- Bulbar weakness with aspiration risk
- Need for intubation
Assessment
Fatigability Tests:
- Sustained upgaze (ptosis after 60 seconds)
- Repeated shoulder abduction
- Count to 50 (voice fatigue)
Ocular:
- Ptosis assessment
- Eye movements (complex ophthalmoplegia)
Bulbar:
- Speech (nasal, fatigable)
- Swallowing assessment
Limbs:
- Proximal power testing
- Neck flexion
Respiratory:
- FVC if any concern
- Single breath count
Antibody Testing
| Antibody | Sensitivity (Generalised) | Sensitivity (Ocular) |
|---|---|---|
| AChR | 85% | 50% |
| MuSK | 5-10% (if AChR negative) | Rare |
| LRP4 | 1-3% | Rare |
Electrophysiology
| Test | Finding |
|---|---|
| Repetitive nerve stimulation (RNS) | Greater than 10% decrement at 3Hz |
| Single-fibre EMG (SF-EMG) | Increased jitter (most sensitive) |
Imaging
| Modality | Indication |
|---|---|
| CT Chest | Thymoma screening (all patients) |
| MRI Chest | If CT equivocal |
Other
- Thyroid function (autoimmune thyroid disease associated)
- PFTs (FVC baseline and monitoring)
- Ice test: Improvement of ptosis with ice application (bedside test)
Algorithm
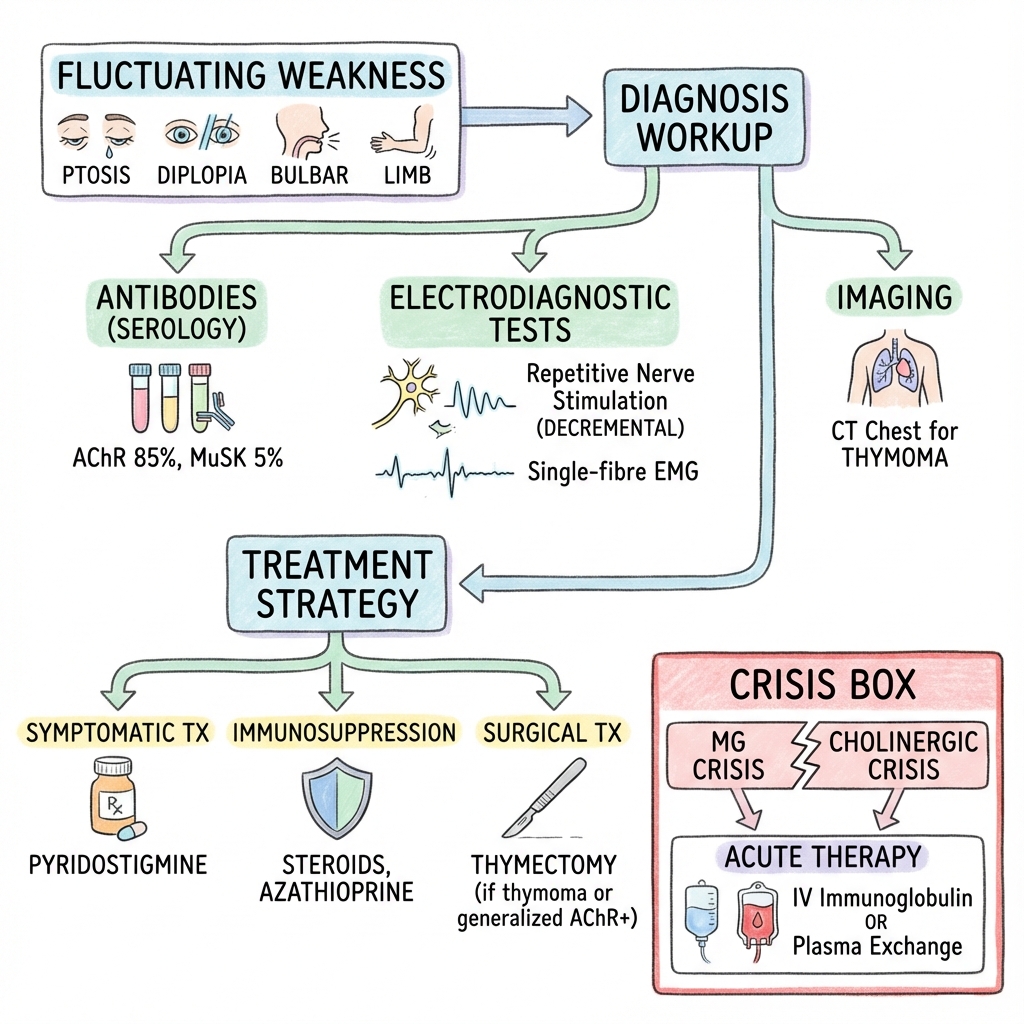
Symptomatic Treatment
| Drug | Dose | Notes |
|---|---|---|
| Pyridostigmine | 30-60mg QDS | Titrate to effect; max 120mg QDS |
Side effects: Cholinergic (diarrhoea, cramps, salivation)
Immunosuppression
| Drug | Dose | Onset | Notes |
|---|---|---|---|
| Prednisolone | Start 10mg, increase slowly to 0.5-1mg/kg | Weeks | Start low to avoid initial worsening |
| Azathioprine | 2-3mg/kg/day | 6-12 months | Steroid-sparing; check TPMT |
| Mycophenolate | 1-1.5g BD | 3-6 months | Alternative to azathioprine |
| Rituximab | 375mg/m2 or 1g x2 | Weeks-months | Especially effective in MuSK-MG |
Thymectomy
| Indication | Notes |
|---|---|
| Thymoma | Mandatory |
| Generalised AChR+ MG, age less than 65 | Recommended (MGTX trial) |
| Ocular MG | Consider if progressing |
| MuSK-MG | Not beneficial |
Myasthenic Crisis
Definition: Respiratory failure requiring ventilation
Management:
- ICU admission
- Stop pyridostigmine (to distinguish from cholinergic crisis)
- Intubate if FVC less than 1L or declining
- Treat with:
- Plasma exchange (PLEX): 5 exchanges over 10-14 days
- OR IVIG: 2g/kg over 5 days
- Identify and treat trigger (infection, drug)
Drugs to AVOID in MG
| Category | Examples |
|---|---|
| Antibiotics | Aminoglycosides, fluoroquinolones, macrolides, tetracyclines |
| Cardiac | Beta-blockers, calcium channel blockers, quinidine |
| Other | Magnesium, D-penicillamine, botulinum toxin |
| Complication | Incidence | Management |
|---|---|---|
| MG crisis | 15-20% | ICU, PLEX/IVIG |
| Aspiration pneumonia | Common if bulbar | Swallow assessment |
| Immunosuppression side effects | Variable | Monitor |
| Thymoma (if present) | May be malignant | Surgical resection |
Outcomes
- With treatment: Near-normal life expectancy
- Mortality: Less than 5% (mainly from crisis/complications)
- Remission: 20-30% achieve medication-free remission
- Generalisation: 50-80% of ocular MG generalises within 2 years
Prognostic Factors
Good:
- Young onset
- Thymic hyperplasia (not thymoma)
- AChR antibody positive
- Early thymectomy
Poor:
- Thymoma
- MuSK-positive
- Late onset
- Delayed diagnosis
Key Guidelines
- AANEM Guidelines — Diagnosis of MG
- International Consensus Guidance (2016) — Treatment of MG PMID: 27207582
Key Trials
MGTX Trial (2016) — Thymectomy improved outcomes in non-thymomatous generalised AChR+ MG. PMID: 27509100
What is Myasthenia Gravis?
Your immune system is attacking the connection between your nerves and muscles. This makes your muscles weak, especially when you use them repeatedly - like by the end of the day.
How is it treated?
We use medications to improve the nerve-muscle connection (pyridostigmine) and medications to calm your immune system. Some people benefit from surgery to remove the thymus gland.
Warning Signs (Crisis)
Go to hospital immediately if:
- Severe breathing difficulty
- Cannot swallow safely
- Rapidly worsening weakness
-
Sanders DB et al. International Consensus Guidance for Management of Myasthenia Gravis. Neurology. 2016;87(4):419-425. PMID: 27207582
-
Wolfe GI et al. Randomized Trial of Thymectomy in Myasthenia Gravis (MGTX). N Engl J Med. 2016;375(6):511-522. PMID: 27509100
-
Gilhus NE et al. Myasthenia gravis. Nat Rev Dis Primers. 2019;5(1):30. PMID: 31048702
-
Juel VC, Massey JM. Myasthenia gravis. Orphanet J Rare Dis. 2007;2:44. PMID: 17986328
-
Evoli A. Myasthenia gravis: new developments in research and treatment. Curr Opin Neurol. 2017;30(5):464-470. PMID: 28763299
Viva Points
"MG is an autoimmune NMJ disorder with fatigable weakness. 85% have AChR antibodies; 5-10% MuSK. Diagnose with antibodies and RNS/SF-EMG. CT chest for thymoma. Treat with pyridostigmine, steroids (start low), thymectomy (MGTX trial). MG crisis: PLEX or IVIG."
Key Facts
- AChR antibodies 85%; MuSK 5-10%
- Thymoma in 10-15%
- Start steroids low (can worsen initially)
- MuSK-MG: bulbar, atrophy, poor pyridostigmine response
- Avoid aminoglycosides, beta-blockers, magnesium
Common Mistakes
- Not starting high-dose steroids abruptly
- Not checking for thymoma
- Missing MuSK testing in seronegative cases
- Prescribing contraindicated drugs
Last Reviewed: 2026-01-01 | MedVellum Editorial Team