Haemophagocytic Lymphohistiocytosis
Summary
Haemophagocytic lymphohistiocytosis (HLH) is a life-threatening syndrome of uncontrolled immune activation characterised by fever, cytopenias, hepatosplenomegaly, and hyperferritinaemia. It occurs when the immune system fails to appropriately terminate an inflammatory response, leading to tissue infiltration by activated macrophages and lymphocytes. HLH can be primary (familial, due to genetic defects in cytotoxic function) or secondary (acquired, triggered by infection, malignancy, or autoimmune disease). Secondary HLH in adults is far more common and termed "reactive HLH" or, when occurring in rheumatic disease, "macrophage activation syndrome (MAS)". Without treatment, HLH is rapidly fatal. Management involves treating the underlying trigger and immunosuppression.
Key Facts
- Definition: Hyperinflammatory syndrome from uncontrolled immune activation
- Incidence: 1-2 per million (likely underdiagnosed)
- Mortality: 40-60% even with treatment; near 100% untreated
- Common Triggers: Viral infection (EBV), malignancy (lymphoma), autoimmune (SLE, Still's)
- Pathognomonic Finding: Hyperferritinaemia greater than 10,000 highly suggestive (sensitivity 95%)
- Gold Standard: HLH-2004 criteria (≥5 of 8)
- First-line Treatment: Treat trigger + immunosuppression (dexamethasone ± etoposide)
- Prognosis: Variable - depends on underlying cause and time to treatment
Clinical Pearls
Diagnostic Pearl: Ferritin greater than 10,000 μg/L is highly suggestive of HLH. Consider the diagnosis in any patient with unexplained fever, cytopenias, and extremely elevated ferritin.
Treatment Pearl: Do not delay immunosuppression while awaiting full workup if HLH suspected - mortality increases with delay.
Pitfall Warning: Haemophagocytosis on marrow is not required for diagnosis and is neither sensitive nor specific alone.
Mnemonic: HLH causes CHAOS - Cytopenias, Hepatosplenomegaly, Aminotransferases elevated, Overwhelming inflammation, Sky-high ferritin
Why This Matters Clinically
HLH is often unrecognised, leading to preventable deaths. It occurs across specialties - haematology, rheumatology, oncology, infectious diseases, ICU. Early recognition and treatment improves survival dramatically.
Incidence
- Estimated 1-2 per million (severe underdiagnosis)
- Primary (familial): 1 in 50,000 children
- Secondary (acquired): More common in adults
Demographics
- Primary: Infancy, early childhood
- Secondary: Any age; median in adults 40-60 years
Triggers for Secondary HLH
| Category | Triggers |
|---|---|
| Infection | EBV (most common), CMV, HIV, influenza, COVID-19 |
| Malignancy | Lymphoma (T-cell, NK-cell), leukaemia |
| Autoimmune | SLE, Still's disease, dermatomyositis (termed MAS) |
| Medication | Checkpoint inhibitors, CAR-T cells |
| Other | Transplant, immunodeficiency |
Mechanism
Step 1: Initiating Trigger
- Infection, malignancy, or autoimmune flare
- In primary HLH: genetic defect in cytotoxic granule function (perforin, Munc13-4)
Step 2: Failed Immune Termination
- Normal: Cytotoxic T-cells/NK cells kill infected/abnormal cells and then terminate response
- HLH: Cytotoxic function impaired → persistent antigen stimulation
Step 3: Cytokine Storm
- Massive release of IFN-γ, IL-1, IL-6, IL-18, TNF-α
- Macrophage hyperactivation
- Systemic inflammation
Step 4: Tissue Infiltration
- Activated macrophages infiltrate organs (liver, spleen, marrow, CNS)
- Haemophagocytosis: Macrophages engulfing blood cells
- Ferritin release from activated macrophages
Step 5: Multi-Organ Failure
- Bone marrow: Cytopenias
- Liver: Hepatitis, coagulopathy
- Spleen: Splenomegaly
- CNS: Encephalopathy, seizures
- Without treatment: Death from MOF
Genetic Causes (Familial HLH)
| Gene | Protein | Function |
|---|---|---|
| PRF1 | Perforin | Pore formation in target cells |
| UNC13D | Munc13-4 | Granule priming |
| STX11 | Syntaxin-11 | Granule fusion |
| STXBP2 | Munc18-2 | Granule docking |
| RAB27A | Rab27a | Granule transport |
Symptoms
Signs
Red Flags
[!CAUTION]
- Ferritin greater than 10,000 μg/L
- Progressive multi-organ failure
- Rapidly falling fibrinogen
- Refractory fever with cytopenias
- Encephalopathy
HLH-2004 Diagnostic Criteria
Diagnosis = ≥5 of 8 criteria:
- Fever ≥38.5°C
- Splenomegaly
- Cytopenias (2+ lineages): Hb less than 90, Platelets less than 100, Neutrophils less than 1.0
- Hypertriglyceridaemia (greater than 3 mmol/L) OR hypofibrinogenaemia (less than 1.5 g/L)
- Haemophagocytosis (marrow, spleen, lymph node)
- Low/absent NK cell activity
- Ferritin 500+ μg/L (but greater than 10,000 highly suggestive)
- Elevated sCD25 (soluble IL-2 receptor) ≥2400 U/mL
H-Score (Probability Calculator)
| Variable | Points |
|---|---|
| Known immunosuppression | Yes: +18 |
| Temperature | less than 38.4: 0; 38.4-39.4: +33; greater than 39.4: +49 |
| Organomegaly | Hepato + spleno: +38; Hepato or spleno: +23 |
| Triglycerides | less than 1.5: 0; 1.5-4: +44; greater than 4: +64 |
| Ferritin | less than 2000: 0; 2000-6000: +35; greater than 6000: +50 |
| AST | less than 30: 0; 30+: +19 |
| Fibrinogen | greater than 2.5: 0; 2.5 or less: +30 |
| Cytopenias | 1: 0; 2: +24; 3: +34 |
| Haemophagocytosis on marrow | Yes: +35 |
Score 169+ = greater than 90% probability of HLH
Laboratory
| Test | Typical Finding |
|---|---|
| Ferritin | Massively elevated (often greater than 10,000) |
| Triglycerides | Elevated |
| Fibrinogen | Low (consumed) |
| LDH | Elevated |
| Transaminases | Elevated |
| Bilirubin | Elevated |
| D-dimer | Elevated |
| sCD25 | Elevated |
| NK cell function | Reduced |
Bone Marrow
- Haemophagocytosis (macrophages engulfing blood cells)
- May be absent early - does not exclude diagnosis
- Rule out malignancy
Imaging
- CT chest/abdomen/pelvis: Splenomegaly, lymphadenopathy, exclude malignancy
- MRI brain if neurological symptoms
Algorithm
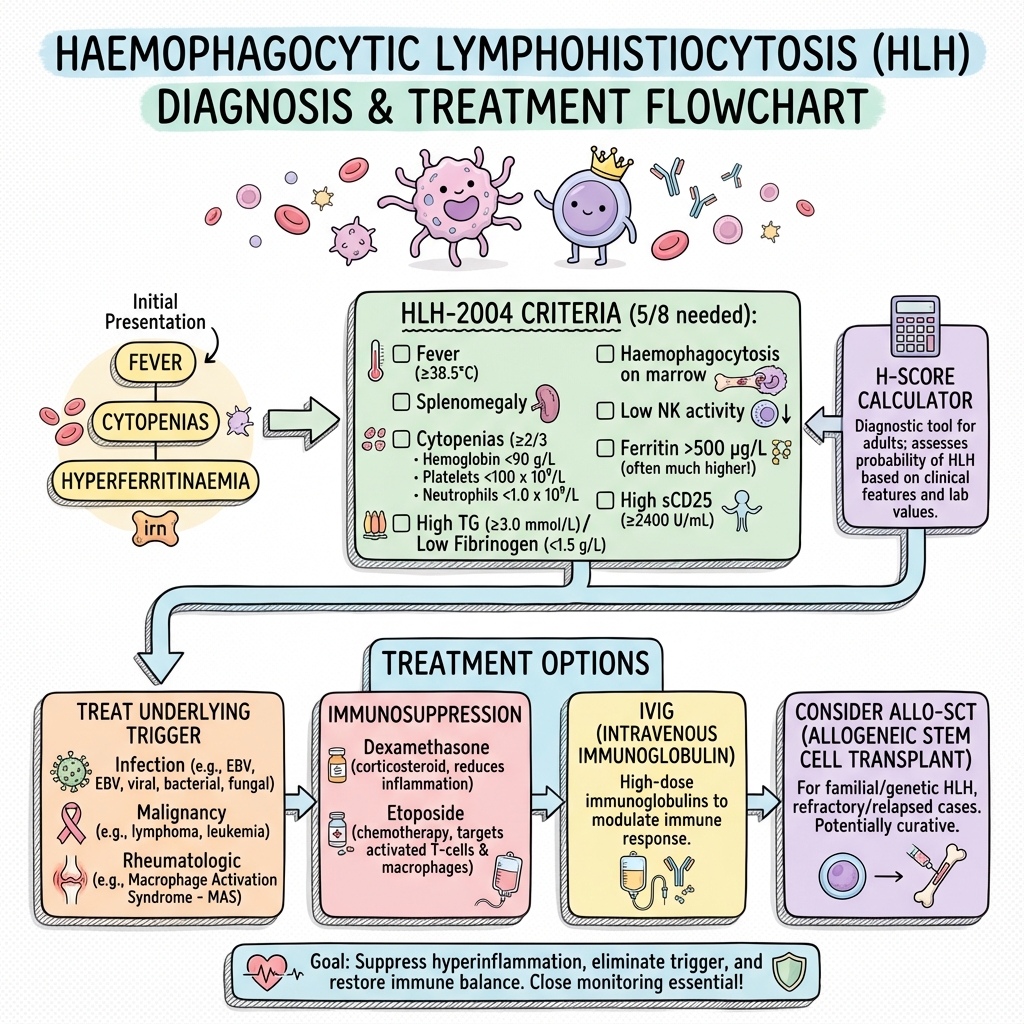
Immediate
- Supportive care (ICU if needed)
- Treat underlying trigger (infection, malignancy)
- Start immunosuppression - do not delay
Treat Underlying Trigger
| Trigger | Treatment |
|---|---|
| Infection (viral) | Antivirals (ganciclovir for CMV, acyclovir for HSV) |
| Malignancy | Appropriate chemotherapy |
| Autoimmune (MAS) | High-dose steroids, anakinra |
Immunosuppression
HLH-94/2004 Protocol:
| Drug | Dose | Notes |
|---|---|---|
| Dexamethasone | 10mg/m² weeks 1-2, then taper | CNS penetration |
| Etoposide | 150mg/m² twice weekly weeks 1-2, then weekly | If severe/no response |
| Ciclosporin | 3mg/kg/day | Added at week 3 in HLH-2004 |
Adult-Modified Approaches:
- May use lower etoposide doses
- Anakinra (IL-1 inhibition) increasingly used, especially for MAS
- Ruxolitinib (JAK inhibitor) emerging therapy
Refractory/Relapsed HLH
- Alemtuzumab
- Emapalumab (anti-IFN-γ) - FDA approved for primary HLH
- Allogeneic stem cell transplant (familial HLH - curative)
Supportive
- Transfusion support
- Infection prophylaxis/treatment
- ICU support for organ failure
| Complication | Incidence | Management |
|---|---|---|
| Multi-organ failure | 50% | ICU, organ support |
| Infection | Common | Broad-spectrum antibiotics |
| CNS involvement | 30% | Intrathecal therapy |
| DIC | Common | FFP, platelets |
| Death | 40-60% | Early treatment |
Outcomes
- Overall mortality: 40-60% (even with treatment)
- Familial HLH: Fatal without SCT
- Infection-triggered: Better prognosis if infection controlled
- Malignancy-triggered: Prognosis linked to malignancy
Prognostic Factors
Poor:
- Delay in diagnosis/treatment
- Malignancy-associated
- CNS involvement
- Lack of response to initial therapy
- EBV-driven HLH
Key Guidelines
- HLH-2004 Protocol — Standard diagnostic and treatment protocol PMID: 17182553
- Histiocyte Society Guidelines — Consensus recommendations
Key Studies
- HLH-94/2004 Trials — Established treatment protocol
- Emapalumab (NICE-301 Trial) — Anti-IFN-γ for primary HLH PMID: 32615408
What is HLH?
HLH is a condition where your immune system becomes overactive and starts damaging your own body. It causes very high fevers, low blood counts, and can affect your liver and other organs.
How is it treated?
We need to treat whatever triggered it (infection, etc.) and use medications to calm down your immune system. Sometimes chemotherapy or special antibody treatments are needed.
-
Henter JI et al. HLH-2004: Diagnostic and therapeutic guidelines. Pediatr Blood Cancer. 2007;48(2):124-131. PMID: 16937360
-
La Rosée P et al. Recommendations for the management of hemophagocytic lymphohistiocytosis in adults. Blood. 2019;133(23):2465-2477. PMID: 30992265
-
Fardet L et al. Development and validation of the HScore. Arthritis Rheumatol. 2014;66(9):2613-2620. PMID: 24782338
-
Locatelli F et al. Emapalumab in Primary Hemophagocytic Lymphohistiocytosis. N Engl J Med. 2020;382(19):1811-1822. PMID: 32615408
Viva Points
"HLH is a hyperinflammatory syndrome of immune dysregulation. Diagnosis requires 5+ of 8 HLH-2004 criteria. Ferritin greater than 10,000 highly suggestive. Treat underlying trigger + immunosuppression (dexamethasone +/- etoposide). Mortality 40-60%."
Key Facts
- Ferritin greater than 10,000 = HLH until proven otherwise
- EBV most common infectious trigger
- MAS = HLH in rheumatic disease context
- Haemophagocytosis not required for diagnosis
Common Mistakes
- ❌ Waiting for haemophagocytosis on marrow
- ❌ Delay in starting immunosuppression
- ❌ Missing the underlying trigger
Last Reviewed: 2026-01-01 | MedVellum Editorial Team