Hereditary Haemochromatosis
Summary
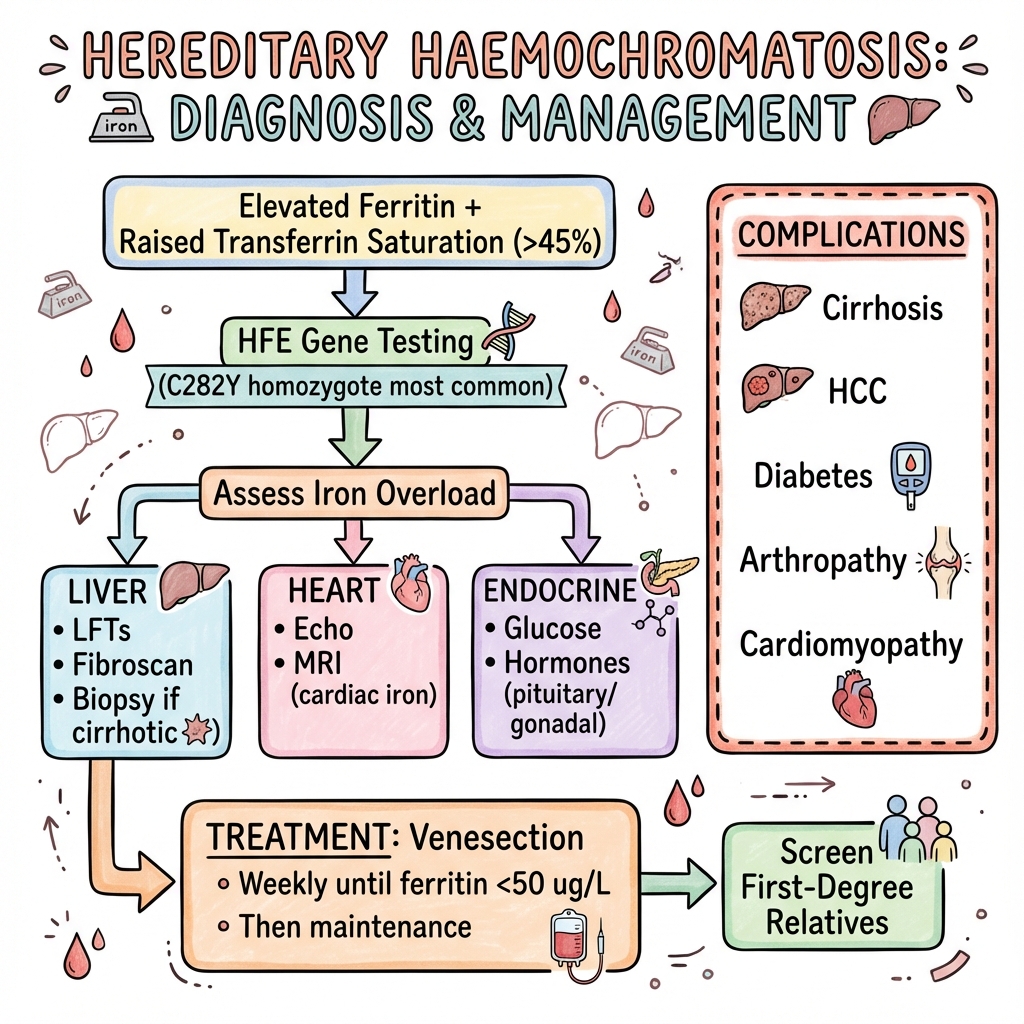
Hereditary haemochromatosis (HH) is an autosomal recessive disorder of iron metabolism resulting in excessive iron absorption and tissue deposition. The most common form is caused by C282Y homozygosity in the HFE gene. Iron accumulates in the liver, heart, pancreas, joints, and endocrine organs, leading to cirrhosis, cardiomyopathy, diabetes, arthropathy, and hypogonadism. Diagnosis is by elevated transferrin saturation and ferritin, confirmed by HFE genotyping. Treatment is venesection (phlebotomy) to remove excess iron. Early diagnosis prevents complications; cirrhosis once established is irreversible.
Key Facts
- Definition: AR disorder of iron metabolism (HFE gene)
- Incidence: 1 in 200-300 (Northern European); low penetrance
- Peak Demographics: Men 40-60; women post-menopause
- Pathognomonic: Transferrin saturation greater than 45% + elevated ferritin + C282Y/C282Y
- Gold Standard Investigation: HFE genotyping
- First-line Treatment: Venesection until ferritin less than 50
- Prognosis: Normal life expectancy if treated before cirrhosis
Clinical Pearls
Diagnostic Pearl: Transferrin saturation is the best screening test. Ferritin can be elevated by inflammation.
Treatment Pearl: Venesect weekly (500ml blood) until ferritin less than 50, then maintain with 3-4 per year.
Screening Pearl: Screen all first-degree relatives with HFE genotyping and iron studies.
Symptoms
"Bronze Diabetes" Triad
Organ Manifestations
| Organ | Manifestation |
|---|---|
| Liver | Hepatomegaly, cirrhosis, HCC |
| Heart | Dilated cardiomyopathy, arrhythmias |
| Pancreas | Diabetes (insulin-dependent) |
| Joints | Arthropathy (especially MCP) |
| Pituitary | Hypogonadism |
| Skin | Pigmentation |
| Test | Finding |
|---|---|
| Transferrin saturation | Greater than 45% (fasting) |
| Ferritin | Elevated (may be very high) |
| HFE genotype | C282Y homozygote (most common) |
| LFTs | May be elevated |
| Liver MRI (R2*) | Quantifies iron deposition |
| Liver biopsy | If cirrhosis suspected |
Algorithm
Venesection
| Phase | Protocol |
|---|---|
| Induction | 450-500ml weekly until ferritin less than 50 |
| Maintenance | Every 2-4 months to maintain ferritin 50-100 |
Monitoring
- Ferritin and Hb before each venesection
- LFTs 6-monthly
- HCC surveillance (AFP, USS 6-monthly if cirrhotic)
- DEXA for osteoporosis
Family Screening
- HFE genotype and iron studies in first-degree relatives
-
European Association for the Study of the Liver. EASL Clinical Practice Guidelines for HFE Hemochromatosis. J Hepatol. 2010;53(1):3-22. PMID: 20471131
-
Bacon BR et al. Diagnosis and Management of Hemochromatosis: 2011 Practice Guideline by AASLD. Hepatology. 2011;54(1):328-343. PMID: 21452290
Viva Points
"Haemochromatosis is AR iron overload (HFE C282Y). Screen with transferrin saturation; confirm with genotype. Complications: cirrhosis, HCC, diabetes, cardiomyopathy, arthropathy. Treat with venesection to ferritin less than 50. Screen relatives."
Last Reviewed: 2026-01-01 | MedVellum Editorial Team