Guillain-Barre Syndrome
Summary
Guillain-Barre syndrome (GBS) is an acute immune-mediated polyradiculoneuropathy characterised by rapidly progressive symmetrical weakness, areflexia, and sensory symptoms. It typically follows a respiratory or gastrointestinal infection (commonly Campylobacter jejuni) by 1-4 weeks. The most common form is acute inflammatory demyelinating polyneuropathy (AIDP). GBS can cause life-threatening respiratory failure and requires close monitoring of respiratory function. CSF shows albumino-cytological dissociation (high protein, normal cells). Treatment with IVIG or plasma exchange hastens recovery. Most patients recover, but 20% have significant residual disability.
Key Facts
- Definition: Acute immune-mediated polyradiculoneuropathy
- Incidence: 1-2 per 100,000 per year
- Peak Demographics: Any age; slight male predominance
- Preceding Infection: 70% (Campylobacter most common)
- Pathognomonic: Ascending weakness + areflexia + albumino-cytological dissociation
- Gold Standard Investigation: CSF (high protein, normal WCC) + NCS
- First-line Treatment: IVIG 0.4g/kg/day x 5 days OR plasma exchange
- Prognosis: 80% recover independently; 5% mortality
Clinical Pearls
Emergency Pearl: Monitor FVC every 4-6 hours. FVC less than 20ml/kg or declining by greater than 30% = consider intubation.
Diagnostic Pearl: CSF may be normal in first week. LP on day 7-10 has higher yield for raised protein.
Treatment Pearl: IVIG and plasma exchange are equally effective. Do NOT give both together or use steroids alone.
Why This Matters Clinically
GBS is a neurological emergency. Respiratory failure can develop rapidly. Early treatment with IVIG or PLEX improves outcomes. ICU admission is often required.
Incidence
- 1-2 per 100,000 per year
- Slight male predominance
- All ages; incidence increases with age
Preceding Infections
| Organism | Frequency | Subtype Association |
|---|---|---|
| Campylobacter jejuni | 30% | AMAN |
| CMV | 10% | AIDP |
| EBV | 10% | AIDP |
| Mycoplasma | 5% | AIDP |
| HIV | Rare | |
| Zika virus | Outbreaks | AIDP |
Mechanism
Step 1: Preceding Infection
- Infection triggers immune response
- Molecular mimicry: Pathogen antigens resemble nerve components
Step 2: Autoimmune Attack
- Antibodies and T cells attack peripheral nerves
- AIDP: Demyelination (Schwann cells attacked)
- AMAN: Axonal damage (ganglioside antibodies)
Step 3: Nerve Dysfunction
- Demyelination causes conduction block
- Weakness, sensory impairment
- Autonomic involvement
Step 4: Nadir and Recovery
- Weakness peaks at 2-4 weeks
- Remyelination and axonal regeneration over months
Subtypes
| Subtype | Features |
|---|---|
| AIDP | Most common (90% in West); demyelinating |
| AMAN | Axonal; associated with Campylobacter |
| AMSAN | Axonal motor and sensory; severe |
| Miller Fisher | Ataxia, areflexia, ophthalmoplegia; anti-GQ1b |
Symptoms
Signs
Red Flags
[!CAUTION]
- Rapidly progressive weakness
- FVC declining or less than 20ml/kg
- Bulbar weakness (aspiration risk)
- Autonomic instability
CSF (Lumbar Puncture)
| Finding | Interpretation |
|---|---|
| Protein | Elevated (may be normal week 1) |
| WCC | Normal (fewer than 10 cells/microL) |
| Pattern | Albumino-cytological dissociation |
Nerve Conduction Studies
| Pattern | Interpretation |
|---|---|
| Prolonged F-wave latencies | Early finding |
| Conduction block | Demyelinating (AIDP) |
| Reduced CMAP | Axonal (AMAN) |
Antibodies
| Antibody | Association |
|---|---|
| Anti-GQ1b | Miller Fisher syndrome |
| Anti-GM1, GD1a | AMAN |
Respiratory Monitoring
- FVC every 4-6 hours
- Rule of 20-30-40: FVC less than 20, MIP less than 30, MEP less than 40 = impending failure
Algorithm
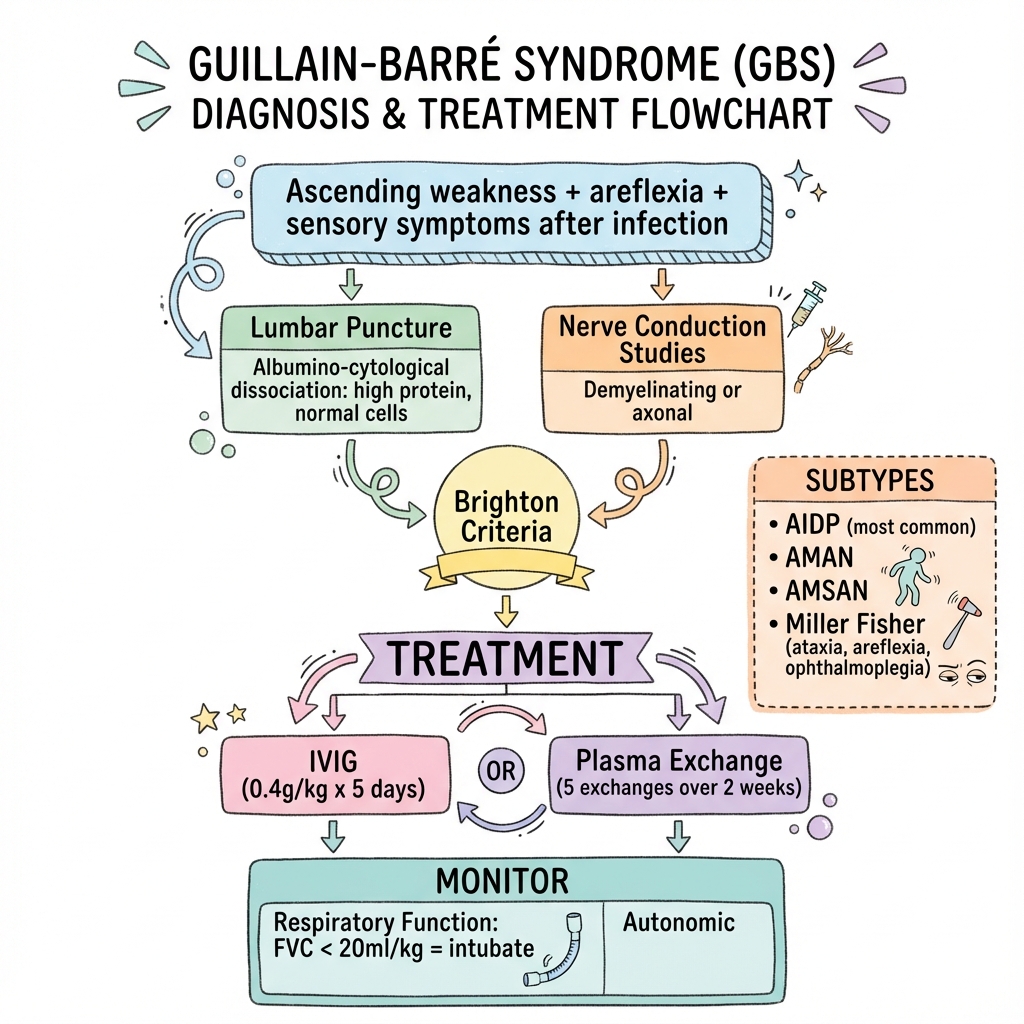
Immunotherapy (Start Early)
| Treatment | Regimen | Notes |
|---|---|---|
| IVIG | 0.4g/kg/day x 5 days | Most commonly used |
| Plasma exchange | 5 exchanges over 10-14 days | Equally effective |
Do NOT:
- Combine IVIG and PLEX (no added benefit)
- Use corticosteroids alone (ineffective)
Respiratory Management
- ICU admission if respiratory concern
- Intubate if FVC less than 20ml/kg or 30% decline
- Mechanical ventilation in 25%
Supportive Care
- DVT prophylaxis
- Physiotherapy
- Pain management (neuropathic pain common)
- Autonomic monitoring (cardiac telemetry)
- Nutritional support
Rehabilitation
- Early physiotherapy
- Prolonged recovery (months to years)
Outcomes
- 80% walk independently at 6 months
- 60% full recovery at 1 year
- 20% significant residual disability
- 5% mortality (respiratory, autonomic, PE)
Poor Prognostic Factors
- Older age
- Preceding Campylobacter infection
- Axonal subtype
- Rapid progression
- Requiring ventilation
-
Willison HJ et al. Guillain-Barre syndrome. Lancet. 2016;388(10045):717-727. PMID: 26948435
-
Hughes RAC et al. Immunotherapy for Guillain-Barre syndrome. Cochrane Database Syst Rev. 2014. PMID: 25238327
-
Van Doorn PA. Guillain-Barre syndrome. Handb Clin Neurol. 2013;117:279-287. PMID: 24095154
Viva Points
"GBS is acute immune-mediated polyradiculoneuropathy. Presents with ascending weakness, areflexia after infection. CSF: high protein, normal cells. Treat with IVIG or plasma exchange. Monitor FVC closely - intubate if less than 20."
Key Facts
- Ascending weakness + areflexia
- Albumino-cytological dissociation
- Campylobacter most common trigger
- Miller Fisher: ataxia, areflexia, ophthalmoplegia + anti-GQ1b
- FVC monitoring critical
Common Mistakes
- Not monitoring respiratory function
- Giving steroids alone
- Missing Miller Fisher variant
Last Reviewed: 2026-01-01 | MedVellum Editorial Team