Cerebral Venous Sinus Thrombosis
Summary
Cerebral venous sinus thrombosis (CVST) is thrombosis of the dural venous sinuses and/or cerebral veins, causing impaired venous drainage, raised intracranial pressure, and potential venous infarction. It is an important cause of stroke in young adults, particularly women (due to hormonal factors). Presentation is variable: isolated intracranial hypertension (headache, papilloedema), focal neurological deficits, seizures, or encephalopathy. Diagnosis requires CT or MR venography. Despite the frequent presence of haemorrhagic infarction, anticoagulation is the mainstay of treatment. With treatment, 80% achieve good outcome, but mortality is 5-10% and recurrence occurs in 5-15%.
Key Facts
- Definition: Thrombosis of cerebral venous sinuses and/or cortical veins
- Incidence: 3-4 per million adults; up to 12 per million including children
- Peak Demographics: Young adults, especially women (F:M 3:1); median age 35 years
- Common Locations: Superior sagittal sinus (60%), transverse sinus (40%), sigmoid sinus
- Pathognomonic: Empty delta sign on CT; absent flow on venography
- Gold Standard Investigation: MR venography (MRV) or CT venography (CTV)
- First-line Treatment: Anticoagulation (LMWH then warfarin/DOAC)
- Prognosis: 80% good outcome; 5-10% mortality; 5-15% recurrence
Clinical Pearls
Diagnostic Pearl: Consider CVST in any young patient with headache and one of: seizures, focal deficit, papilloedema, or risk factors (OCP, pregnancy, thrombophilia).
Treatment Pearl: Anticoagulation is safe and recommended even with haemorrhagic venous infarction - haemorrhage is secondary to venous congestion.
Pitfall Warning: Normal CT brain does NOT exclude CVST - venography (CTV or MRV) is required.
Mnemonic: CVST - Combined oral Contraceptive, Venogram needed, Safe to anticoagulate, Thrombophilia workup
Why This Matters Clinically
CVST is a treatable cause of stroke and raised ICP in young adults. Delay in diagnosis leads to preventable morbidity and mortality. Awareness of risk factors and low threshold for venographic imaging is essential.
Incidence
- Adults: 3-4 per million per year
- Neonates: Higher incidence (venous thrombosis more common)
- Female predominance: 75% (hormonal factors)
Risk Factors
| Category | Factors |
|---|---|
| Hormonal | OCP (most common acquired risk), pregnancy, postpartum, HRT |
| Thrombophilia | Factor V Leiden, prothrombin G20210A, protein C/S deficiency, antithrombin deficiency, antiphospholipid syndrome |
| Infection | Mastoiditis, sinusitis, meningitis (septic CVST) |
| Inflammatory | IBD, Behçet's disease, SLE, sarcoidosis |
| Malignancy | Haematological and solid tumours |
| Mechanical | Head trauma, neurosurgery, lumbar puncture |
| Haematological | Polycythaemia, sickle cell, thrombocytosis |
| Medication | L-asparaginase, tamoxifen |
Mechanism
Step 1: Thrombus Formation
- Virchow's triad: Stasis, endothelial injury, hypercoagulability
- Risk factors alter coagulation balance
- Thrombus forms in dural sinus (most commonly superior sagittal)
Step 2: Impaired Venous Drainage
- CSF absorption impaired (arachnoid granulations drain into sinuses)
- Raised intracranial pressure
- Venous congestion in draining territories
Step 3: Venous Infarction
- Backpressure causes capillary damage
- Vasogenic oedema
- Petechial haemorrhage → haemorrhagic infarction (characteristic)
- May progress to larger haemorrhage
Step 4: Clinical Manifestations
- Raised ICP: Headache, papilloedema, 6th nerve palsy
- Venous infarction: Focal deficits, seizures
- Cerebral oedema: Encephalopathy, coma
Step 5: With Treatment
- Anticoagulation prevents thrombus propagation
- Recanalisation occurs over weeks-months
- New venous collaterals develop
Sites Affected
| Sinus | Frequency | Clinical Features |
|---|---|---|
| Superior sagittal | 60% | Bilateral deficits, ICP, seizures |
| Transverse | 40% | Headache, lateral signs, mastoid tenderness |
| Sigmoid | 20% | Similar to transverse |
| Cavernous | less than 5% | Orbital pain, chemosis, CN III/IV/VI palsies |
| Deep cerebral veins | 10% | Severe: bilateral thalamic, coma |
Symptoms
Signs
Presentation Patterns
| Pattern | Features |
|---|---|
| Isolated intracranial hypertension | Headache, papilloedema, no focal signs |
| Focal syndrome | Deficits ± seizures |
| Encephalopathy | Diffuse dysfunction, coma |
| Cavernous sinus syndrome | Orbital pain, chemosis, ophthalmoplegia |
Red Flags
[!CAUTION]
- Thunderclap headache
- Headache with seizure
- Headache + focal deficit in young adult
- Headache in pregnancy/postpartum
- Headache + OCP use + smoking
- Deteriorating consciousness
Neurological Assessment
General:
- GCS assessment
- Signs of meningism (may occur)
Eyes:
- Fundoscopy: Papilloedema
- Eye movements: 6th nerve palsy
- Visual acuity
Motor/Sensory:
- Focal deficits (often bilateral if sagittal sinus)
- Upper motor neuron signs
Local:
- Mastoid tenderness (lateral sinus from mastoiditis)
- Facial swelling (cavernous sinus)
Imaging
| Modality | Findings | Role |
|---|---|---|
| CT Brain | May be normal; "delta sign" (empty triangle in sagittal sinus); hyperdense sinus; haemorrhagic infarction | Initial screening |
| CT Venography | Filling defect in sinus; gold standard for acute diagnosis | Diagnostic |
| MR Venography | Flow void absence; gold standard | Diagnostic |
| MRI Brain | Venous infarction pattern; sinus signal abnormality | Parenchymal assessment |
 MRI showing venous infarction. Source: Wikipedia Commons (CC-BY)
MRI showing venous infarction. Source: Wikipedia Commons (CC-BY)
 Axial T1 MRI showing sinus thrombosis. Source: Wikipedia Commons (CC-BY-SA)
Axial T1 MRI showing sinus thrombosis. Source: Wikipedia Commons (CC-BY-SA)
Laboratory
| Test | Purpose |
|---|---|
| FBC | Polycythaemia, thrombocytosis |
| Coagulation screen | Baseline for anticoagulation |
| D-dimer | May be elevated; low sensitivity, useful if low clinical suspicion |
| Thrombophilia screen | Factor V Leiden, prothrombin mutation, protein C/S, antithrombin (do AFTER acute phase) |
| Antiphospholipid antibodies | Lupus anticoagulant, anticardiolipin, anti-β2GP1 |
| Pregnancy test | Exclude pregnancy |
Lumbar Puncture
- Opening pressure often elevated (greater than 25 cmH2O)
- CSF may be normal or show raised protein, mild pleocytosis
- Do NOT perform if mass effect or haemorrhage on imaging
Algorithm
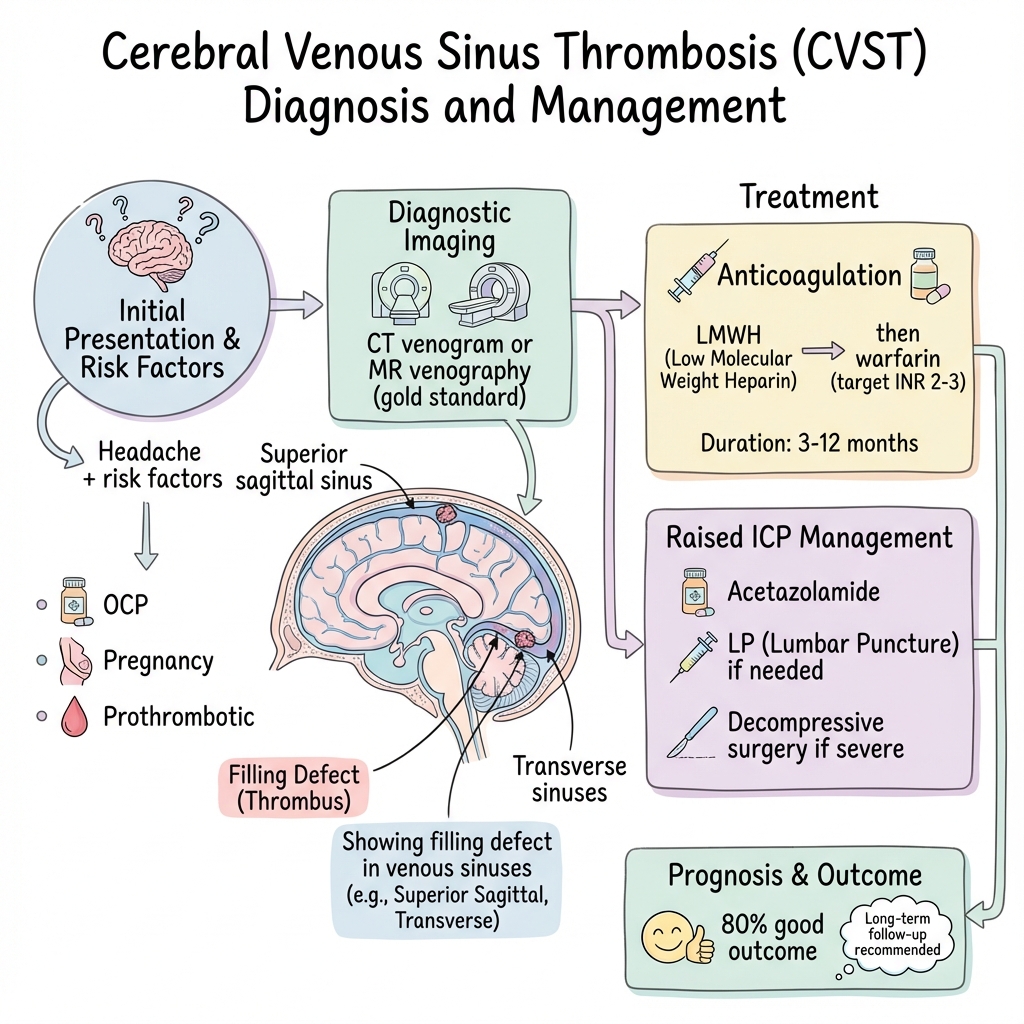
Anticoagulation (Mainstay)
Acute Phase:
- LMWH (e.g., enoxaparin 1mg/kg BD) - preferred
- UFH if high bleeding risk or procedure anticipated
- Safe even with haemorrhagic infarction
Transition:
- Warfarin (INR 2-3) OR DOAC (evidence emerging for DOACs)
Duration:
| Scenario | Duration |
|---|---|
| Provoked (reversible risk e.g., OCP, infection) | 3-6 months |
| Unprovoked or mild thrombophilia | 6-12 months |
| Severe thrombophilia or recurrent | Lifelong |
Management of Raised ICP
- Head elevation 30°
- Acetazolamide (reduces CSF production)
- Therapeutic LP if idiopathic intracranial hypertension features
- Repeat LP if visual threatened
- Decompressive craniectomy if malignant oedema
Seizure Management
- Treat seizures acutely (lorazepam, levetiracetam)
- Prophylactic anticonvulsants not routinely recommended
Endovascular Treatment
- Reserved for deterioration despite anticoagulation
- Mechanical thrombectomy
- Local thrombolysis (limited evidence)
Remove/Treat Underlying Cause
- Stop OCP
- Treat infection if septic CVST
- Manage underlying prothrombotic condition
Disposition
- Admit: All confirmed CVST - neurology/stroke unit
- ICU: Coma, large haemorrhage, requiring ICP monitoring
- Follow-up: Neurology, imaging at 3-6 months, consider haematology
| Complication | Incidence | Management |
|---|---|---|
| Haemorrhagic infarction | 30-40% | Continue anticoagulation |
| Seizures | 40% | Anticonvulsants |
| Visual loss (papilloedema) | 5-10% permanent | Acetazolamide, LP, shunt |
| Hydrocephalus | Rare | VP shunt |
| Death | 5-10% | Prevention, aggressive treatment |
| Recurrence | 5-15% | Depends on underlying risk |
Outcomes
- Complete recovery: 80%
- Moderate-severe disability: 10-15%
- Death: 5-10%
- Recurrence: 5-15% (higher if persistent risk factor)
Prognostic Factors
Good:
- Young age
- Alert at presentation
- Isolated headache syndrome
- No haemorrhage
- Lateral sinus thrombosis
Poor:
- Coma at presentation
- Deep venous system thrombosis
- Haemorrhage with mass effect
- Malignancy-associated
- Septic CVST
Key Guidelines
- AHA/ASA Guidelines: CVST (2011) — PMID: 21293023
- European Stroke Organisation Guidelines (2017) — Updated recommendations
- NICE Stroke Guidelines — General stroke management applicable
Key Studies
TO-ACT Trial (2020) — Did not show benefit of endovascular treatment over anticoagulation alone in most patients. PMID: 32798216
ISCVT Study (2004) — Largest prospective CVST cohort establishing outcomes and prognostic factors. PMID: 14970229
What is CVST?
A blood clot forms in the veins that drain blood from your brain. This raises pressure inside your head and can damage brain tissue.
How serious is it?
It's serious and needs urgent treatment. With treatment, most people (80%) make a good recovery.
Treatment
Blood thinners (anticoagulation) to stop the clot growing and help your body dissolve it. You'll need blood thinners for several months.
Warning Signs
Return to hospital if:
- Worsening headache
- Vision changes
- Seizures
- Weakness or numbness
-
Saposnik G et al. Diagnosis and Management of Cerebral Venous Thrombosis: A Statement for Healthcare Professionals. Stroke. 2011;42(4):1158-1192. PMID: 21293023
-
Ferro JM et al. ISCVT Investigators. Prognosis of Cerebral Vein and Dural Sinus Thrombosis. Stroke. 2004;35(3):664-670. PMID: 14976332
-
Coutinho JM et al. TO-ACT Investigators. Effect of Endovascular Treatment on Medical Outcomes in Cerebral Venous Thrombosis. JAMA Neurol. 2020;77(8):966-973. PMID: 32364579
-
Stam J. Thrombosis of the Cerebral Veins and Sinuses. N Engl J Med. 2005;352(17):1791-1798. PMID: 15858188
-
Bousser MG, Ferro JM. Cerebral venous thrombosis: An update. Lancet Neurol. 2007;6(2):162-170. PMID: 17239803
Viva Points
"CVST is thrombosis of cerebral venous sinuses, presenting with headache, seizures, or focal deficits. Common in young women (OCP, pregnancy). Diagnose with CT/MR venography. Anticoagulate even if haemorrhagic - this is venous congestion. 80% good outcome."
Key Facts
- F:M 3:1, median age 35
- OCP most common acquired risk factor
- Anticoagulation safe despite haemorrhage
- Normal CT does NOT exclude - need venography
Common Mistakes
- ❌ Stopping anticoagulation due to haemorrhagic infarction
- ❌ Not requesting venography (normal CT doesn't exclude)
- ❌ Missing in pregnancy/postpartum headache
- ❌ Forgetting thrombophilia workup
Last Reviewed: 2026-01-01 | MedVellum Editorial Team