Autoimmune Encephalitis
Summary
Autoimmune encephalitis (AE) is a group of inflammatory brain disorders caused by antibodies against neuronal cell surface or synaptic proteins. Previously underrecognised, AE is now known to be as common as infectious encephalitis and is a treatable cause of cognitive decline, seizures, and psychiatric symptoms. The most common subtype is anti-NMDA receptor encephalitis, typically affecting young women and associated with ovarian teratoma. Other important antibodies include anti-LGI1, anti-CASPR2, anti-GABAb, and anti-AMPAR. Diagnosis relies on clinical features, MRI (often showing mesial temporal signal change), CSF pleocytosis, and specific antibody testing. Treatment involves first-line immunotherapy (steroids, IVIG, plasma exchange) and second-line agents (rituximab, cyclophosphamide). With treatment, 80% improve, though recovery may take months.
Key Facts
- Definition: Immune-mediated encephalitis caused by antibodies targeting neuronal antigens
- Incidence: 5-8 per million per year; as common as infectious encephalitis
- Peak Demographics: Anti-NMDAR young women (15-35); Anti-LGI1 older adults (50-70)
- Associated Tumours: Ovarian teratoma (anti-NMDAR ~50% of women), SCLC (anti-GABAb), thymoma (anti-CASPR2)
- Gold Standard Investigation: Neuronal antibody panel (serum AND CSF)
- First-line Treatment: IV methylprednisolone, IVIG, plasma exchange
- Prognosis: 80% improve with treatment; 20-25% relapse
Clinical Pearls
Diagnostic Pearl: "New-onset refractory status epilepticus (NORSE) in a young person should prompt immediate AE workup and empirical immunotherapy."
Treatment Pearl: Start immunotherapy early - delays in treatment worsen outcome. Do not wait for antibody results.
Pitfall Warning: Anti-NMDAR encephalitis often presents to psychiatry first. Any young patient with new psychosis should be screened.
Mnemonic: NMDAR - New psychosis, Movement disorder, DAyslong seizures, Autonomic instability, Resembles schizophrenia
Why This Matters Clinically
AE is treatable and reversible, but outcomes depend on early diagnosis and immunotherapy. Psychiatric manifestations mean patients often present to mental health services first. Recognition is essential for neurologists, psychiatrists, and acute physicians.
Incidence
- Overall AE: 5-8 per million per year
- Anti-NMDAR encephalitis: ~1.5 per million (most common)
- Anti-LGI1: ~0.8 per million
Demographics by Antibody
| Antibody | Age | Sex | Tumour Association |
|---|---|---|---|
| Anti-NMDAR | 15-35 | F > M (4:1) | Ovarian teratoma (50% F) |
| Anti-LGI1 | 50-70 | M > F (2:1) | Rare (thymoma) |
| Anti-CASPR2 | 40-70 | M > F (10:1) | Thymoma (20%) |
| Anti-GABAb | 50-70 | M = F | SCLC (50%) |
| Anti-AMPAR | 50-70 | F > M | SCLC, thymoma, breast |
Mechanism
Step 1: Trigger Event
- Often unknown trigger
- Viral prodrome may precede (HSV encephalitis can trigger anti-NMDAR)
- Tumour expresses neuronal antigen (teratoma contains neural tissue)
Step 2: Loss of Immune Tolerance
- B-cell activation against neuronal surface antigens
- Antibody production (IgG)
- Antibodies cross blood-brain barrier or produced intrathecally
Step 3: Antibody-Mediated Neuronal Dysfunction
- Antibodies bind to synaptic receptors/proteins
- Receptor internalisation or cross-linking
- Disrupted neurotransmission (NOT cell death initially - hence reversible)
- Examples: NMDAR internalisation → NMDA hypofunction (psychosis, movement disorder)
Step 4: Clinical Syndrome
- Limbic symptoms: Memory impairment, confusion, psychiatric
- Seizures: Often focal, may progress to status
- Movement disorders: Dyskinesias, catatonia, rigidity
- Autonomic: Instability, hypoventilation
- Decreased consciousness
Step 5: With Treatment
- Immunotherapy removes/neutralises antibodies
- Receptor expression recovers
- Clinical improvement (may take months)
- Tumour removal essential if present
Antibody Classification
| Type | Antibodies | Mechanism |
|---|---|---|
| Cell surface | NMDAR, LGI1, CASPR2, GABAb, AMPAR | Pathogenic; good response |
| Intracellular | Hu, Yo, Ri, ANNA-1 | Paraneoplastic; T-cell mediated; poor response |
By Antibody
Anti-NMDAR Encephalitis:
Anti-LGI1 Encephalitis:
Anti-CASPR2:
Anti-GABAb:
Red Flags
[!CAUTION]
- Rapid cognitive decline over days-weeks
- New-onset refractory seizures
- Young person with first psychotic episode
- Movement disorder + encephalopathy
- Autonomic instability
- Faciobrachial dystonic seizures
Assessment
Cognitive:
- Mini-mental state, MoCA
- Short-term memory impairment
Psychiatric:
- Screen for psychosis, mood symptoms
- Catatonia (mutism, posturing, waxy flexibility)
Neurological:
- Seizures
- Movement disorder (choreoathetosis, dyskinesia)
- Cerebellar signs
- Autonomic: HR, BP variability
General:
- Tumour search: Pelvic (ovary), chest (lung), thymus
Antibody Testing
| Antibody | Order | Notes |
|---|---|---|
| Anti-NMDAR | Serum AND CSF | CSF more sensitive |
| Anti-LGI1 | Serum (CSF less reliable) | Often serum-only positive |
| Anti-CASPR2 | Serum | May be low titre |
| Anti-GABAb | Serum AND CSF | |
| Anti-AMPAR | Serum AND CSF | |
| Paraneoplastic panel | Serum | Hu, Yo, Ri, CV2, amphiphysin |
CSF
| Finding | Comments |
|---|---|
| Lymphocytic pleocytosis | 80% (typically 10-100 WBC) |
| Elevated protein | 30-50% |
| Oligoclonal bands | 60% |
| Normal glucose | Usually normal |
Imaging
| Modality | Findings |
|---|---|
| MRI Brain | Mesial temporal T2/FLAIR hyperintensity (60-70%); may be normal |
| FDG-PET | More sensitive than MRI; frontotemporal hypometabolism |
EEG
- Diffuse slowing
- Epileptiform discharges
- Extreme delta brush (anti-NMDAR specific)
- Faciobrachial dystonic seizures may not have ictal correlate
Tumour Screening
| Antibody | Imaging |
|---|---|
| Anti-NMDAR | MRI/USS pelvis (ovarian teratoma) |
| Anti-GABAb, AMPAR | CT chest (SCLC) |
| Anti-CASPR2, Hu | CT chest (thymoma, SCLC) |
| All | Consider PET-CT if no tumour found |
Algorithm
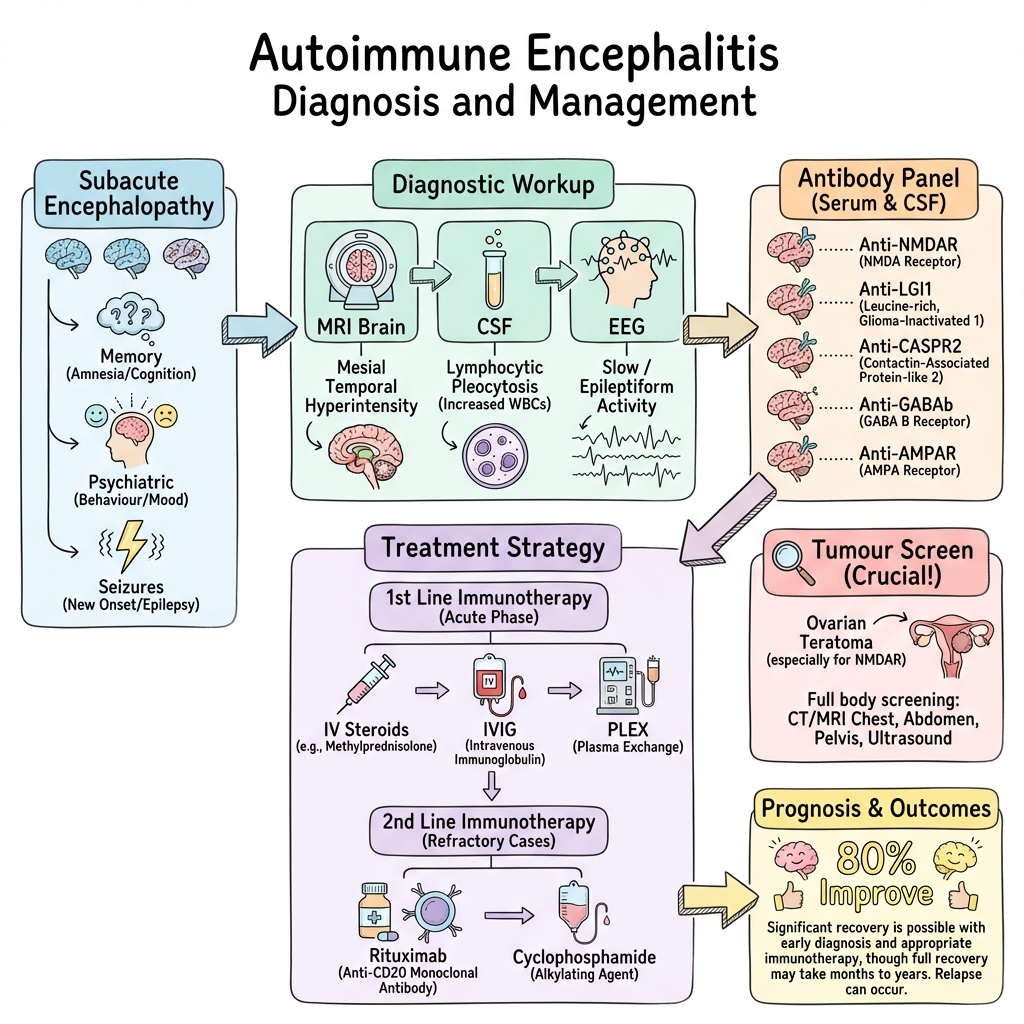
Diagnostic Approach
Use clinical diagnostic criteria:
- Subacute onset (less than 3 months) of memory deficit, altered mental status, or psychiatric symptoms
- At least one of: New focal CNS findings, seizures, CSF pleocytosis, MRI limbic encephalitis
- Reasonable exclusion of alternative causes
First-Line Immunotherapy
Start empirically if clinical suspicion high - do not wait for antibodies
| Treatment | Dose | Notes |
|---|---|---|
| IV Methylprednisolone | 1g daily for 5 days | Followed by oral taper |
| IVIG | 0.4g/kg daily for 5 days | Or divided over 2-5 days |
| Plasma exchange | 5-7 exchanges | Alternative to IVIG |
Second-Line Immunotherapy
If inadequate response to first-line (usually assessed at 2-4 weeks):
| Treatment | Dose | Notes |
|---|---|---|
| Rituximab | 375mg/m² weekly x4, OR 1g x2 | Most commonly used |
| Cyclophosphamide | 750mg/m² monthly x6 | Alternative |
Tumour Management
- Essential if paraneoplastic
- Tumour removal improves outcome and reduces relapse
- Screen repeatedly if initially negative (up to 5 years for NMDAR)
Seizure Management
- Anti-seizure medications (levetiracetam, clobazam, lacosamide)
- Often refractory until immunotherapy works
Supportive Care
- ICU for autonomic instability, hypoventilation, refractory seizures
- Psychiatry involvement
- Physiotherapy, OT for rehabilitation
Long-Term Management
- Maintenance immunotherapy (rituximab every 6 months) may reduce relapse
- Monitor for tumour development
- Neuropsychological follow-up
| Complication | Incidence | Management |
|---|---|---|
| Status epilepticus | 30-40% | Aggressive AEDs, immunotherapy, ICU |
| Respiratory failure | 20% (NMDAR) | Ventilation |
| Autonomic crisis | 20% | ICU monitoring |
| Cognitive impairment | 30% long-term | Rehabilitation |
| Relapse | 20-25% (NMDAR) | Maintenance immunotherapy |
| Death | 5-10% | Early treatment, tumour removal |
Outcomes
- 80% improve with treatment
- Full recovery: 50-60%
- Some disability: 20-30%
- Severe disability/death: 10-20%
Prognostic Factors
Good:
- Early treatment
- Tumour identified and removed
- Anti-LGI1 (excellent response)
- Younger age
Poor:
- ICU admission
- Delayed treatment
- Intracellular antibodies (Hu, Yo)
- No tumour found but expected (missed tumour)
- Anti-NMDAR without teratoma (may have longer course)
Key Guidelines
- Lancet Neurology Consensus Criteria (2016) — Graus et al. Diagnostic criteria for autoimmune encephalitis. PMID: 26906964
- Practice Guidelines (2021) — AAN recommendations
Key Studies
Dalmau et al. (2007) — Original description of anti-NMDAR encephalitis. PMID: 17270458
Titulaer et al. (2013) — Treatment and prognostic factors in 577 anti-NMDAR cases. PMID: 23295932
What is Autoimmune Encephalitis?
Your immune system has made antibodies that are attacking your brain by mistake. This causes problems with memory, behaviour, seizures, and movement.
How is it treated?
We use medications to calm down your immune system and stop the antibodies attacking your brain. Most people get better, but it can take weeks to months.
Warning Signs
- Return of confusion or seizures
- New symptoms
-
Graus F et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15(4):391-404. PMID: 26906964
-
Dalmau J et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis. Lancet Neurol. 2008;7(12):1091-1098. PMID: 18851928
-
Titulaer MJ et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis. Lancet Neurol. 2013;12(2):157-165. PMID: 23295932
-
Irani SR et al. Faciobrachial dystonic seizures precede Lgi1 antibody limbic encephalitis. Ann Neurol. 2011;69(5):892-900. PMID: 21416487
-
Lancaster E et al. Antibodies to the GABA(B) receptor in limbic encephalitis. Neurology. 2010;75(3):224-228. PMID: 20644152
Viva Points
"Autoimmune encephalitis is antibody-mediated brain inflammation. Anti-NMDAR is commonest, affecting young women, associated with ovarian teratoma. Presents with psychosis, seizures, movement disorder. Treat early with steroids, IVIG, PLEX; second-line rituximab. 80% improve."
Key Facts
- Anti-NMDAR: young women, teratoma, psychosis + movement disorder
- Anti-LGI1: older adults, faciobrachial dystonic seizures, hyponatraemia
- Start immunotherapy empirically - don't wait for results
- Tumour removal essential if present
Common Mistakes
- ❌ Missing diagnosis in "psychiatric" presentation
- ❌ Waiting for antibody results before treating
- ❌ Not searching for tumour
- ❌ Stopping immunotherapy too early
Last Reviewed: 2026-01-01 | MedVellum Editorial Team