Antiphospholipid Syndrome
Summary
Antiphospholipid syndrome (APS) is an acquired autoimmune thrombophilia characterised by arterial and/or venous thrombosis and/or pregnancy morbidity in the presence of persistent antiphospholipid antibodies (aPL). It is the most common acquired cause of thrombophilia. APS can be primary (isolated) or secondary (associated with SLE or other autoimmune diseases). The three clinically relevant aPL are lupus anticoagulant (LA), anticardiolipin antibodies (aCL), and anti-β2-glycoprotein I antibodies (anti-β2GPI). Diagnosis requires clinical criteria (thrombosis or pregnancy morbidity) plus laboratory criteria (persistent aPL positivity on two occasions ≥12 weeks apart). Management involves anticoagulation for thrombotic APS and aspirin ± LMWH for obstetric APS. Catastrophic APS (CAPS) is a rare, life-threatening variant with rapid multi-organ failure.
Key Facts
- Definition: Autoimmune thrombophilia with aPL causing thrombosis and/or pregnancy morbidity
- Incidence: 2-5 per 100,000; 30-40% of SLE patients have aPL
- Peak Demographics: Women 20-40 years (especially obstetric APS); M:F 1:5
- Common Manifestations: DVT/PE (most common), stroke, recurrent miscarriage
- Pathognomonic: Persistent aPL + thrombosis or pregnancy morbidity
- Gold Standard: Revised Sapporo (Sydney) classification criteria
- First-line Treatment: Warfarin INR 2-3 (thrombotic); Aspirin + LMWH (obstetric)
- Prognosis: Good with anticoagulation; high recurrence without treatment
Clinical Pearls
Diagnostic Pearl: aPL must be positive on TWO occasions, at least 12 weeks apart, to confirm diagnosis - transient positivity is common.
Treatment Pearl: DOACs are generally NOT recommended in APS - warfarin remains standard. Triple-positive patients especially should avoid DOACs.
Pitfall Warning: Lupus anticoagulant causes prolonged APTT but is associated with THROMBOSIS, not bleeding.
Mnemonic: APS - Antibodies (aPL), Pregnancy loss, (thrombo)Sis
Why This Matters Clinically
APS is the most common acquired thrombophilia. It explains many cases of "unexplained" thrombosis in young patients and recurrent pregnancy loss. Recognition guides lifelong anticoagulation decisions.
Incidence and Prevalence
- APS: 2-5 per 100,000 per year
- aPL positivity in general population: 1-5%
- aPL positivity in SLE: 30-40%
Demographics
| Factor | Details |
|---|---|
| Age | 20-40 years typical; can occur at any age |
| Sex | F:M 5:1 (especially obstetric APS) |
| Ethnicity | All ethnicities; may be higher in Caucasians |
Primary vs Secondary APS
| Type | Definition |
|---|---|
| Primary APS | APS without underlying autoimmune disease |
| Secondary APS | APS associated with SLE or other autoimmune disease |
Mechanism
Step 1: Antiphospholipid Antibody Production
- Autoantibodies target phospholipid-binding proteins (especially β2-glycoprotein I)
- Trigger unknown; may be molecular mimicry, infection, genetic predisposition
Step 2: Endothelial Activation
- aPL bind to β2GPI on endothelial cells
- Activation of endothelium → procoagulant state
- Increased tissue factor expression
Step 3: Platelet Activation
- aPL bind to platelets via β2GPI
- Platelet activation and aggregation
- Enhanced thrombin generation
Step 4: Complement Activation
- Complement pathway activation contributes to thrombosis
- Particularly important in pregnancy morbidity
Step 5: Thrombosis
- Arterial or venous thrombosis
- Any vascular bed can be affected
- Recurrence without treatment
Pregnancy Morbidity Mechanism
- Placental thrombosis and infarction
- Anti-β2GPI affects trophoblast function
- Complement-mediated placental damage
- Leads to miscarriage, IUGR, pre-eclampsia
Triple Positivity
Highest risk when positive for all three:
- Lupus anticoagulant (LA)
- Anticardiolipin (aCL)
- Anti-β2GPI
Thrombotic Manifestations
| Site | Manifestation |
|---|---|
| Venous | DVT (most common), PE, cerebral vein thrombosis, renal vein |
| Arterial | Stroke, TIA, MI, peripheral arterial thrombosis |
| Microvascular | Livedo reticularis, skin necrosis, renal TMA |
Obstetric Manifestations
Other Features
Catastrophic APS (CAPS)
Red Flags
[!CAUTION]
- Stroke or MI in young patient
- Recurrent venous thrombosis
- ≥3 miscarriages
- Multi-organ failure (CAPS)
- Thrombosis in unusual site
Assessment
Skin:
- Livedo reticularis (legs, trunk)
- Skin ulcers
- Digital gangrene
Cardiovascular:
- Signs of DVT (leg swelling)
- Pulmonary hypertension (if chronic PE)
- Cardiac murmurs (valve disease)
Neurological:
- Focal deficits (stroke)
- Cognitive impairment
Obstetric history:
- Pattern of pregnancy losses
- Complications (pre-eclampsia)
Antiphospholipid Antibody Testing
| Test | Positive Threshold |
|---|---|
| Lupus anticoagulant (LA) | Positive by clotting assay |
| Anticardiolipin IgG | >40 GPL or >99th percentile |
| Anticardiolipin IgM | >40 MPL or >99th percentile |
| Anti-β2GPI IgG | >99th percentile |
| Anti-β2GPI IgM | >99th percentile |
Must be positive on 2 occasions, ≥12 weeks apart
Classification Criteria (Revised Sapporo/Sydney 2006)
Clinical Criteria (≥1):
- Vascular thrombosis (arterial, venous, or small vessel)
- Pregnancy morbidity (as defined above)
Laboratory Criteria (≥1, on 2 occasions ≥12 weeks apart):
- Lupus anticoagulant
- Anticardiolipin IgG or IgM (medium-high titre)
- Anti-β2GPI IgG or IgM
Definite APS = ≥1 clinical + ≥1 laboratory criteria
Other Investigations
| Test | Purpose |
|---|---|
| FBC | Thrombocytopenia |
| Coagulation | APTT prolonged (LA effect) |
| ANA, dsDNA | Exclude SLE |
| Complement (C3, C4) | May be low in SLE-APS |
| Imaging | Confirm thrombosis (Doppler, CT, MRI) |
Algorithm
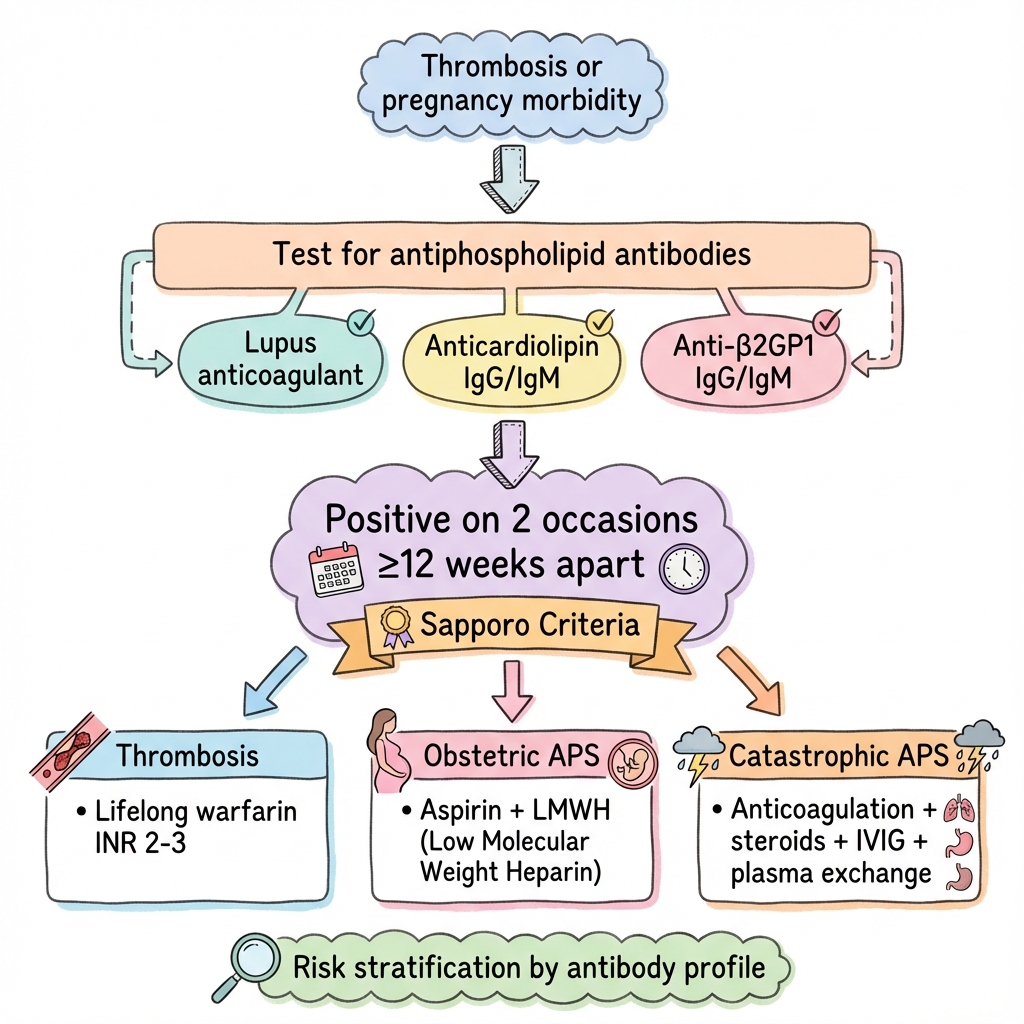
Thrombotic APS
| Scenario | Treatment |
|---|---|
| First venous thrombosis | Warfarin INR 2-3 (lifelong) |
| First arterial thrombosis | Warfarin INR 2-3 + consider aspirin |
| Recurrent thrombosis on warfarin | Increase INR target to 3-4, OR add aspirin, OR switch to LMWH |
DOACs NOT recommended - TRAPS and ASTRO-APS trials showed higher thrombosis rates with rivaroxaban in triple-positive APS
Obstetric APS
| Scenario | Treatment |
|---|---|
| Recurrent early miscarriage | Low-dose aspirin + prophylactic LMWH |
| Late pregnancy loss | Low-dose aspirin + therapeutic LMWH |
| Prior thrombosis + pregnancy | Therapeutic LMWH throughout pregnancy |
| Refractory obstetric APS | Add hydroxychloroquine, steroids, IVIG |
Primary Prevention (aPL Positive, No Thrombosis)
- Low-dose aspirin in high-risk (triple positive, SLE)
- Hydroxychloroquine (especially if SLE)
- Cardiovascular risk factor modification
Catastrophic APS (CAPS)
Emergency treatment:
- Anticoagulation (heparin)
- High-dose corticosteroids
- Plasma exchange or IVIG
- +/- Rituximab, eculizumab in refractory cases
| Complication | Incidence | Management |
|---|---|---|
| Recurrent thrombosis | 10-30%/year without treatment | Lifelong anticoagulation |
| Stroke | 15-20% of APS patients | Secondary prevention |
| CAPS | less than 1% | Aggressive multimodal treatment |
| Pregnancy loss | 50-80% without treatment | Aspirin + LMWH |
| Pulmonary hypertension | 3-4% | Screen, treat |
Outcomes
- With appropriate anticoagulation: Low recurrence (2-5%/year)
- Without treatment: 50-70% recurrence
- Obstetric APS with treatment: 70-80% live birth rate
- CAPS mortality: 30-50%
Prognostic Factors
High Risk:
- Triple positivity (LA + aCL + anti-β2GPI)
- High-titre antibodies
- SLE association
- Prior arterial thrombosis
Key Guidelines
- EULAR Recommendations (2019) — Management of APS PMID: 31092436
- ACR/EULAR Classification Criteria (2023) — Updated criteria PMID: 37587095
Key Trials
TRAPS Trial (2018) — Rivaroxaban inferior to warfarin in triple-positive APS. PMID: 29929950
PREGNANTS Study — Treatment strategies for obstetric APS
What is APS?
Your immune system makes antibodies that increase the risk of blood clots. This can cause clots in your legs, lungs, or brain, or problems during pregnancy.
How is it treated?
Blood thinners (usually warfarin) to prevent clots. If you're planning pregnancy, we use different medications that are safe in pregnancy.
Lifelong considerations
- Take warfarin regularly and have INR monitored
- Avoid factors that increase clot risk
- Inform all doctors about your diagnosis
-
Tektonidou MG et al. EULAR recommendations for the management of antiphospholipid syndrome. Ann Rheum Dis. 2019;78(10):1296-1304. PMID: 31092436
-
Pengo V et al. Rivaroxaban vs warfarin in high-risk patients with antiphospholipid syndrome (TRAPS). Blood. 2018;132(13):1365-1371. PMID: 29929950
-
Miyakis S et al. International consensus statement on an update of the classification criteria for APS (Sydney). J Thromb Haemost. 2006;4(2):295-306. PMID: 16420554
-
Barbhaiya M et al. 2023 ACR/EULAR APS Classification Criteria. Arthritis Rheumatol. 2023;75(10):1687-1702. PMID: 37587095
-
Asherson RA et al. Catastrophic antiphospholipid syndrome (CAPS). J Autoimmun. 2009;33(1):4-8. PMID: 19233595
Viva Points
"APS is an autoimmune thrombophilia with aPL causing thrombosis and pregnancy morbidity. Diagnose with Sapporo criteria: clinical event + persistent aPL (≥12 weeks apart). Treat thrombotic APS with warfarin INR 2-3 (NOT DOACs). Obstetric APS: aspirin + LMWH."
Key Facts
- Three aPL: LA, aCL, anti-β2GPI
- Persistent positivity required (2 tests, 12 weeks apart)
- DOACs contraindicated (especially triple positive)
- Triple positivity = highest risk
- CAPS: multi-organ thrombosis, high mortality
Common Mistakes
- ❌ Using DOACs in APS
- ❌ Diagnosing on single positive aPL test
- ❌ Missing obstetric history in workup
- ❌ Not screening for SLE
Last Reviewed: 2026-01-01 | MedVellum Editorial Team