Aortic Dissection
Summary
Aortic dissection is a tear in the intimal layer of the aorta, allowing blood to enter the media and create a false lumen. It is a cardiovascular emergency with mortality of 1-2% per hour if untreated. Classic presentation is sudden severe "tearing" chest or back pain. Stanford Type A (involving ascending aorta) requires emergency surgery; Type B (descending only) is usually managed medically. Diagnosis is by CT aortic angiogram. Immediate BP and HR control are essential.
Key Facts
- Mechanism: Intimal tear → blood dissects into media → false lumen
- Presentation: Sudden severe chest/back pain, "tearing" quality
- Stanford Type A: Involves ascending aorta — emergency surgery
- Stanford Type B: Descending aorta only — usually medical management
- Imaging: CT aortic angiogram is gold standard
- Mortality: 1-2% per hour untreated (Type A)
Clinical Pearls
Aortic dissection mimics MI — but D-dimer is elevated, and thrombolysis would be fatal
Check BP in BOTH arms — asymmetry over 20 mmHg strongly suggests dissection
Type A mortality = 1-2% per hour untreated — time to diagnosis and surgery is critical
Why This Matters Clinically
Aortic dissection is rapidly fatal if missed. It can mimic many conditions (MI, stroke, PE). All clinicians must recognise the red flags and escalate immediately.
Image Integration Plan
| Asset Type | Source | Status | License |
|---|---|---|---|
| Pathophysiology flowchart | AI-generated (sketchnote) | COMPLETE | N/A |
| Management algorithm | AI-generated (sketchnote) | COMPLETE | N/A |
| CT angiogram dissection flap | Radiopaedia | PENDING | CC-BY-NC-SA |
| CXR widened mediastinum | Wikimedia Commons | PENDING | CC-BY-SA |
Management Algorithm
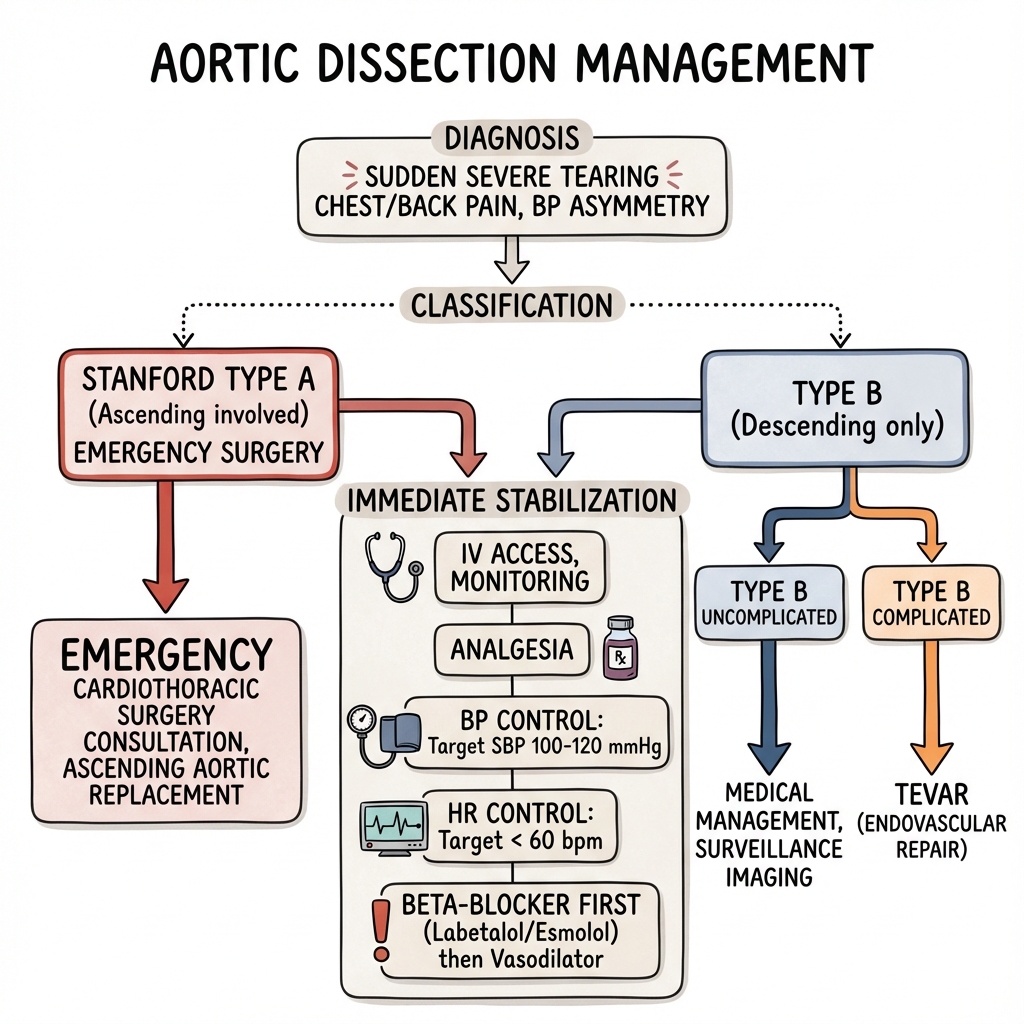
Figure 1: Emergency management algorithm for aortic dissection including BP/HR control and surgical decision-making based on Stanford type.
Pathophysiology Flowchart
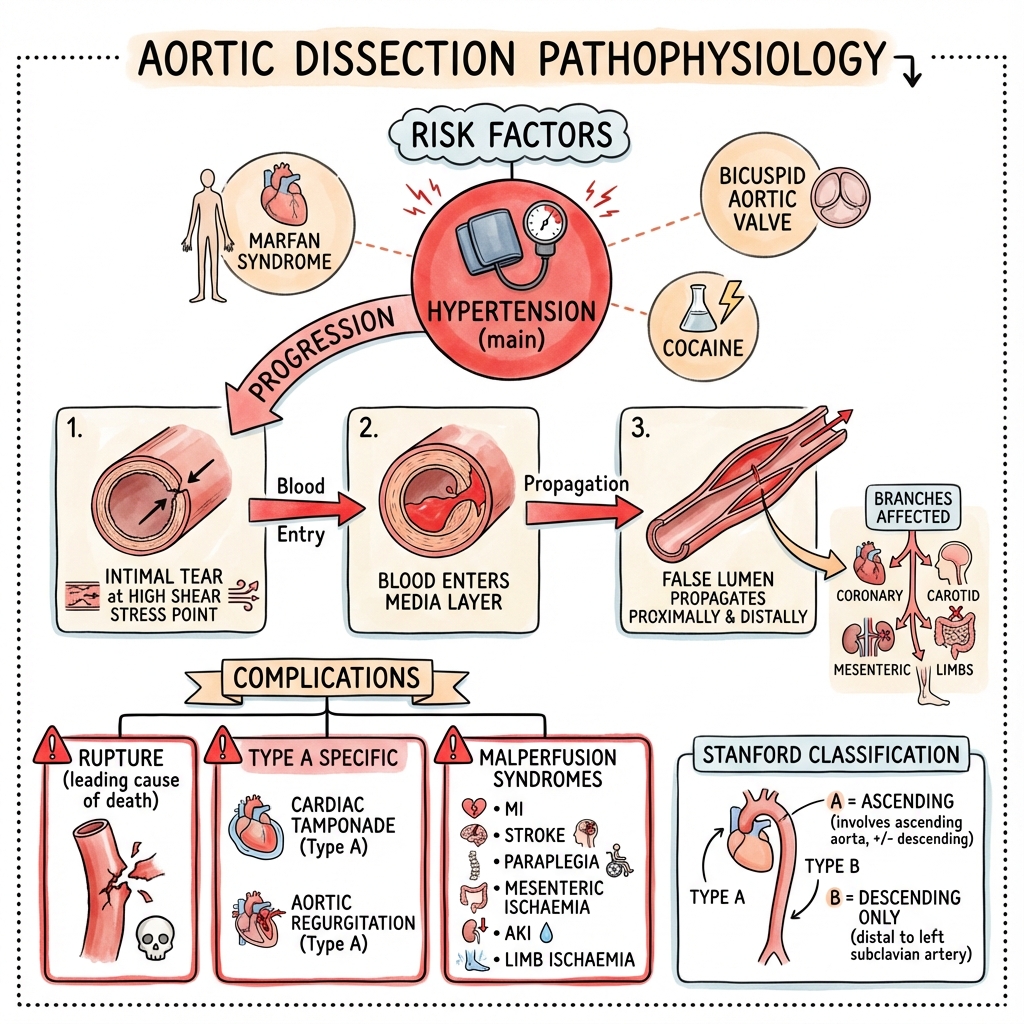
Figure 2: Pathophysiological cascade from intimal tear to false lumen propagation and end-organ malperfusion.
Incidence
- 5-30 per million/year
- Peak age: 60-70 years
- Male:female = 2:1
Risk Factors
| Factor | Notes |
|---|---|
| Hypertension | Most common risk factor (70-80%) |
| Bicuspid aortic valve | Associated with ascending aortopathy |
| Marfan syndrome | FBN1 mutation; aortic root dilatation |
| Ehlers-Danlos type IV | Vascular fragility |
| Turner syndrome | Aortic coarctation, bicuspid valve |
| Cocaine use | Hypertensive crisis precipitant |
| Previous aortic surgery | Anastomosis vulnerability |
| Pregnancy | Third trimester/post-partum |
| Iatrogenic | Catheterisation, surgery |
Mechanism
- Intimal tear (usually at points of maximal shear stress)
- Blood enters media → creates false lumen
- False lumen propagates proximally and/or distally
- Complications: Rupture, malperfusion, aortic regurgitation
Sites of Intimal Tear
- Ascending aorta (65%) — just above aortic valve
- Aortic arch (10%)
- Proximal descending aorta (20%) — just distal to left subclavian
- Distal aorta (5%)
Malperfusion Syndromes
- Coronary: MI (usually RCA → inferior MI)
- Cerebral: Stroke
- Spinal cord: Paraplegia
- Mesenteric: Bowel ischaemia
- Renal: AKI
- Limb: Acute limb ischaemia
Aortic Regurgitation (Type A)
- Dissection disrupts aortic valve commissures
- Acute severe AR → pulmonary oedema
Classic Features
| Feature | Frequency |
|---|---|
| Chest pain | 85-90% |
| Back pain | 50% (interscapular) |
| Sudden onset | 85% |
| Severe intensity | "Worst ever" |
| Tearing/ripping quality | 50% |
| Migratory pain | Follows dissection |
Associated Features
Red Flags
| Finding | Significance |
|---|---|
| Sudden severe pain | Vascular catastrophe |
| Tearing quality | Classic for dissection |
| Pulse/BP asymmetry | Subclavian involvement |
| New AR murmur | Ascending involvement |
| Neurological deficit | Malperfusion |
| Hypotension | Rupture or tamponade |
Vital Signs
- Check BP in BOTH arms (greater than 20 mmHg asymmetry suggestive)
- Hypertension (common) or hypotension (shock/tamponade)
- Tachycardia
Cardiovascular
- Early diastolic murmur (aortic regurgitation) — Type A
- Muffled heart sounds (tamponade)
- Absent/reduced pulses (malperfusion)
- Pulsus paradoxus (tamponade)
Neurological
- Stroke signs (carotid involvement)
- Paraplegia (spinal cord ischaemia)
- Horner syndrome (sympathetic involvement)
Abdominal
- Signs of mesenteric ischaemia
- Renal bruit
Immediate
| Test | Purpose |
|---|---|
| ECG | Exclude MI; may show ischaemia if coronary malperfusion |
| CXR | Widened mediastinum (not always present); pleural effusion |
| Troponin | May be elevated (malperfusion or type 2 MI) |
| D-dimer | Elevated in dissection (helps differentiate from MI) |
| FBC, U&E, coagulation | Baseline |
Definitive Imaging — CT Aortic Angiogram
- Gold standard
- Shows intimal flap, true/false lumen, extent
- Entry and exit tears
- Branch vessel involvement
- Complications (rupture, tamponade)
Other Imaging
| Modality | Role |
|---|---|
| TTE | Ascending aorta, AR, pericardial effusion |
| TOE | High sensitivity for ascending/descending aorta |
| MRI | Excellent accuracy but less available in emergency |
Stanford Classification (Most Clinically Useful)
| Type | Definition | Management |
|---|---|---|
| Type A | Involves ascending aorta (regardless of entry site) | Emergency surgery |
| Type B | Distal to left subclavian only | Medical (unless complicated) |
DeBakey Classification
| Type | Description |
|---|---|
| I | Originates in ascending, propagates to arch/descending |
| II | Confined to ascending aorta |
| IIIa | Descending thoracic aorta only |
| IIIb | Descending thoracic and abdominal aorta |
Complicated vs Uncomplicated Type B
| Complicated | Features |
|---|---|
| Malperfusion | Limb, renal, mesenteric, spinal |
| Rupture | Haemothorax, mediastinal haematoma |
| Refractory pain | Despite adequate analgesia and BP control |
| Rapid expansion | Imaging evidence |
Immediate Stabilisation
- IV access, monitoring
- Analgesia (IV morphine)
- BP control: Target SBP 100-120 mmHg
- HR control: Target under 60 bpm
- Beta-blocker first (labetalol, esmolol) — reduces shear stress
- Then vasodilator if needed (GTN, sodium nitroprusside)
NEVER give vasodilator before beta-blocker — reflex tachycardia increases shear stress
Type A Dissection — Emergency Surgery
- Cardiothoracic surgery consultation immediately
- Ascending aortic replacement ± aortic root/valve
- Mortality 20-30% with surgery (vs over 50% without)
Type B Dissection — Uncomplicated
| Intervention | Details |
|---|---|
| Medical management | BP control, HR control, pain management |
| Surveillance imaging | Repeat CT at 48-72h, then serial |
| Long-term BP | Target under 130/80 |
Type B Dissection — Complicated
| Intervention | Details |
|---|---|
| TEVAR | Thoracic endovascular aortic repair for malperfusion, impending rupture |
| Open surgery | If TEVAR not feasible |
Long-Term Management
- Lifelong BP control (beta-blocker based)
- Serial imaging (CT/MRI) — 6 months, then annually
- Genetic testing if connective tissue disorder suspected
- Family screening
Of Dissection
- Aortic rupture (leading cause of death)
- Cardiac tamponade (Type A)
- Aortic regurgitation (Type A)
- Malperfusion syndromes (MI, stroke, paraplegia, mesenteric ischaemia, AKI, limb ischaemia)
Of Treatment
- Surgical mortality (20-30% for Type A)
- Stroke
- Paraplegia (spinal cord ischaemia)
- Renal failure
- Endoleak (after TEVAR)
Type A Dissection
| Management | Mortality |
|---|---|
| Emergency surgery | 20-30% |
| No surgery | 50-70% at 1 week |
Type B Dissection
| Type | 30-Day Mortality |
|---|---|
| Uncomplicated (medical) | 10% |
| Complicated | 30-50% |
Long-Term
- Surveillance for aneurysm development
- Re-dissection risk
- Late complications at repair site
Key Guidelines
- ESC/EACTS Guidelines on Aortic Diseases (2014, updated)
- ACC/AHA Thoracic Aortic Disease Guidelines (2022)
Key Evidence
- Early surgery improves survival in Type A
- BP and HR control reduce extension and rupture risk
- TEVAR has improved outcomes in complicated Type B
What is Aortic Dissection?
Aortic dissection is a tear in the wall of the main blood vessel from the heart (aorta). It is an emergency that needs urgent treatment.
Symptoms
- Sudden, severe chest or back pain
- Pain described as "tearing" or "ripping"
- Feeling faint
- Different blood pressure in each arm
Treatment
- Medication to lower blood pressure and heart rate
- Surgery to repair the aorta (for some types)
- Keyhole repair with a stent (in some cases)
After Treatment
- Lifelong blood pressure control
- Regular scans to monitor the aorta
- Family members may need screening
Resources
Primary Guidelines
- Erbel R, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases. Eur Heart J. 2014;35(41):2873-2926. PMID: 25173340
- Isselbacher EM, et al. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease. J Am Coll Cardiol. 2022;80(24):e223-e393. PMID: 36334952
Key Studies
- Nienaber CA, et al. Randomized comparison of strategies for type B aortic dissection (INSTEAD). Circulation. 2009;120(25):2519-2528. PMID: 19996018